This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.
A rattlesnake bite delivers venom that can kill within hours, yet some people have walked away from untreated bites and lived to tell about it. The survival odds depend on a narrow set of variables—snake species, venom load, bite location, and how fast your body fights back.
Most untreated victims face tissue death, internal bleeding, and organ failure that antivenom could prevent. The question isn’t whether you can survive without treatment, but whether you’re willing to gamble with your life when effective medical care exists.
Understanding what happens after a bite, how quickly venom spreads, and why some outcomes defy expectations can help you make smarter decisions if you ever find yourself face-to-face with a rattler.
Table Of Contents
- Key Takeaways
- Can You Survive a Rattlesnake Bite Without Treatment?
- How Deadly is Rattlesnake Venom?
- What Happens After a Rattlesnake Bite?
- Which Factors Affect Survival Without Treatment?
- How Long Can You Survive Without Medical Help?
- What First Aid Can Help if No Treatment is Available?
- Can First Aid Alone Save You?
- What Are The Chances of Permanent Injury or Disability?
- Are There Natural Remedies or Home Treatments?
- Why is Immediate Medical Care Critical?
- Frequently Asked Questions (FAQs)
- How long does it take for rattlesnake venom to kill?
- Can sucking out the venom from a bite help?
- Are baby rattlesnakes more dangerous than adult ones?
- What should you do if bitten while hiking alone?
- Can rattlesnake antivenin cause allergic reactions in some people?
- How long can you survive without antivenom treatment?
- What percentage of rattlesnake bites are fatal?
- Do all rattlesnake bites inject venom?
- How quickly does rattlesnake venom spread?
- Can children survive rattlesnake bites better?
- Conclusion
Key Takeaways
- You can survive a rattlesnake bite without treatment, but mortality jumps from under 1% with medical care to 5-25% untreated, with survival hinging on species (Mojave rattlesnakes hit 30-40% lethality), venom load, bite location, and your baseline health.
- Skipping antivenom invites tissue death, internal bleeding, organ failure, and long-term disability—43% of survivors report chronic pain, 37% develop kidney problems, and up to 25% face limb loss or nerve damage that never fully heals.
- First aid like immobilizing the limb and staying calm can slow venom spread by 30-40% temporarily, but it won’t neutralize toxins or prevent systemic damage—antivenom remains the only definitive treatment that stops venom in its tracks.
- Folk remedies like tourniquets, cutting the wound, sucking venom, or applying ice actively worsen outcomes by trapping toxins, destroying tissue, or delaying real care when every hour counts toward preventing irreversible harm.
Can You Survive a Rattlesnake Bite Without Treatment?
Yes, you can survive a rattlesnake bite without treatment, but it’s a dangerous gamble with odds that shift dramatically based on several key factors. Some people have lived through untreated bites, though many suffered serious complications that could have been prevented.
If you’re curious about the risks and realities of handling venomous snakes in general, keeping rattlesnakes as pets involves similar life-or-death considerations that shouldn’t be taken lightly.
Understanding what influences survival helps you grasp why medical care matters so much.
Factors Influencing Survival Odds
Survival odds hinge on several interrelated variables that determine whether you’ll walk away or face life-threatening complications. Understanding these factors helps you gauge the real danger:
- Venom potency and the snake species—Mojave rattlesnakes carry neurotoxins with 30–40% lethality rates untreated, while others range 10–20%
- Bite severity including depth and location near arteries
- Victim profile—age over 40, diabetes, or heart disease sharply raise your risk
Documented Cases of Untreated Survival
You’ll find scattered historical accounts of untreated rattlesnake bite survival in rural recoveries and wilderness survival stories. These rare cases usually involve minimal venom delivery, brief exposure, or unusual venom resistance in otherwise healthy adults.
Still, these cases don’t mean rattlesnakes are safe to ignore—most bites demand immediate medical care, and it’s worth knowing which rattlesnake species are protected by law before you even consider confronting one.
Case reports document full recovery within days to weeks after snakebite events without antivenom, though survival rates in such untreated outcomes remain exceedingly low and unpredictable.
Understanding what to do when a snake bites can dramatically improve outcomes even when antivenom isn’t immediately available.
Risks of Forgoing Medical Care
While rare untreated survival cases exist, skipping emergency medical care dramatically worsens outcomes. Medical delay carries serious consequences:
- Tissue necrosis spreads, often requiring surgery or amputation
- Coagulopathy progresses, risking internal hemorrhage
- Organ failure becomes more likely without antivenom
- Hospital stays extend considerably
- Long-term disability rates climb steeply
Bite severity and venom resistance vary wildly—gambling on survival rates without treatment outcomes data isn’t worth your limb or life.
How Deadly is Rattlesnake Venom?
Not all rattlesnake venom is created equal. The danger you face depends on which species bit you, how much venom entered your body, and what that venom does once it’s in your system.
Let’s break down what makes rattlesnake venom deadly—and why some bites are far worse than others.
Venom Toxicity by Species
Not all rattlesnake species pack the same punch. The Eastern Diamondback delivers large venom yields with potent hemotoxins that destroy tissue, while the Mojave rattlesnake’s neurotoxins can paralyze your respiratory muscles—up to 30-40% lethality untreated. Species variance matters because venom composition and toxicity levels directly determine bite severity and your odds of survival.
If you’re trying to compare toxicity across venomous species, understanding coral snake venom potency reveals how neurotoxic bites differ from the hemotoxic rattlesnake strikes described above.
| Rattlesnake Species | Venom Composition | Toxicity/Lethality |
|---|---|---|
| Eastern Diamondback | High-yield hemotoxins | 10-20% untreated |
| Western Diamondback | Moderate hemotoxins | 10-20% untreated |
| Mojave Rattlesnake | Potent neurotoxins | 30-40% untreated |
| Tiger Rattlesnake | Low venom injection | Lower lethality |
| Arizona/Horned Rattlesnake | Small fangs, less venom | Lower risk |
Amount of Venom Injected
Venom dosage varies wildly—Western diamondback rattlesnakes usually inject 0.5 to 1.5% of their body mass per bite, but extreme cases can approach 1000 mg. Bite severity depends on how much toxin actually enters your body:
- Fang penetration depth determines envenomation rates and venom injection volume
- Multiple strikes greatly increase total snake venom delivered
- Venom yield correlates with individual rattlesnake size and defensive state
- Peak toxin effects usually hit within 1-4 hours after the bite
Effects on The Human Body
Your body’s reaction to rattlesnake bite venom toxicity unfolds fast—cellular destruction starts within minutes as metalloproteinases attack tissue at the site. Snake venom effects quickly spiral: blood coagulation fails, clotting times stretch dangerously, and organ failure threatens kidneys and heart.
Neurological damage may cause facial paralysis or breathing trouble, pushing lethality rates higher without urgent intervention. Understanding snake venom components is essential in treating such bites.
What Happens After a Rattlesnake Bite?
The first minutes and hours after a rattlesnake bite can feel like watching a storm roll in—you know something serious is happening, and the timeline matters. What starts as sharp pain and immediate swelling can quickly spiral into life-threatening complications if the venom isn’t stopped.
Here’s what actually unfolds in your body when treatment isn’t available.
Without treatment, venom spreads through tissue and blood, causing swelling, bleeding, or paralysis depending on the types of snakes involved.
Immediate Symptoms and Progression
Within minutes of a rattlesnake bite, you’ll notice fang punctures and sharp, burning pain at the site—often the first alarm. Swelling usually appears within 30 to 60 minutes and can progress aggressively over the next two to three hours.
Early venom effects include redness, bruising, and tightness as rattlesnake venom toxicity damages blood vessels and soft tissues. Understanding snake bite symptoms is vital for prompt medical treatment.
Severe Complications and Organ Damage
If you don’t get emergency care, the snake venom can trigger catastrophic organ failure within hours. Around 14 to 31 percent of rattlesnake bite victims develop renal dysfunction, and severe coagulopathy may cause life-threatening bleeding. Here’s what you’re facing:
- Blood coagulation breakdown leading to uncontrolled hemorrhage
- Cardiac damage from shock and possible neurotoxin effects
- Acute kidney injury requiring dialysis or causing permanent impairment
That’s why toxin management and emergency care aren’t optional—they’re survival essentials.
Long-Term Effects Without Treatment
Surviving without treatment doesn’t mean walking away unscathed. Forty-three percent of rattlesnake bite survivors report chronic pain, nerve damage, and stiffness years later. Tissue necrosis can scar permanently, and about 3 percent face long-term disability—muscle wasting, joint contractures, even amputation.
Organ failure during the acute phase may progress to kidney disease requiring dialysis. The survival rate improves with toxin management, but skipping care invites lasting consequences.
Which Factors Affect Survival Without Treatment?
Your odds of surviving a rattlesnake bite without treatment aren’t the same for everyone. Several key factors determine whether you’ll pull through or face serious complications.
Let’s break down what actually influences your chances when medical help isn’t available.
Rattlesnake Species and Venom Type
Not all rattlesnakes carry the same punch—some inject venom that’s far deadlier than others, and knowing which species bit you can mean the difference between a painful week and a fight for your life.
Mojave rattlesnakes pack neurotoxins that can paralyze you, hitting 30-40% lethality untreated. Eastern diamondbacks deliver massive venom loads with tissue-destroying hemotoxins.
Meanwhile, Arizona species inject less venom through smaller fangs—still dangerous, but your odds improve.
Bite Location and Depth
Where venom enters your body makes all the difference. A rattlesnake bite to your hand or ankle (distal extremity) usually means slower venom spread and less tissue damage. But if the bite lands near your torso or deep into muscle, envenomation risk and wound severity skyrocket—raising the lethality rate.
- Sudden swelling creeps toward your trunk
- Muscle compartments can suffocate from pressure
- Airway bites threaten breathing within minutes
Victim’s Age and Health Status
Your body’s baseline resilience shapes how rattlesnake venom affects you. Children under 20 can deteriorate faster, while adults over 65 face higher complication rates, including coagulopathy and kidney damage. Chronic conditions like heart disease or renal impairment worsen outcomes, amplifying mortality rates without medical attention. Even healthy individuals aren’t immune: venom sensitivity varies, making professional rattlesnake bite treatment non-negotiable.
| Age Group | Key Health Risks |
|---|---|
| Under 20 | Faster symptom progression, heightened venom sensitivity |
| 18–59 (healthy) | Lower lethality rate with prompt care |
| 65+ | Coagulopathy, renal impairment, cardiac instability |
| Chronic conditions | Nephrotoxicity, delayed toxin clearance, elevated mortality |
How Long Can You Survive Without Medical Help?
The clock starts ticking the moment venom enters your body, but there’s no single answer to how long you have. Your timeline depends on which rattlesnake bit you, how much venom you received, and what shape you’re in when it happens.
Let’s break down what determines your window of survival.
Timeframe for Onset of Severe Symptoms
Within minutes to a few hours after a rattlesnake bite, severe symptoms typically emerge—though some bites deteriorate in just 1–2 hours. Local swelling and pain usually escalate within 30 minutes to 2 hours, signaling venom spread.
Early systemic signs like dizziness or nausea may appear within 1–3 hours. Delayed onset beyond 4 hours is uncommon but still demands urgent emergency response.
Variation by Snake Species and Venom Load
The amount of venom injected—the venom load—varies dramatically by rattlesnake species and even individual snake size. Mojave rattlesnakes deliver potent neurotoxins with a 30–40% lethality rate untreated, while smaller species like the Arizona rattlesnake inject less venom and cause milder bites.
Venom composition also shifts geographically within the same species, affecting bite severity and how quickly symptoms progress.
Survival Timelines in Case Studies
Case analysis shows your survival timelines vary wildly depending on bite severity and venom effects. Here’s what documented snakebite records reveal:
- Mild envenomation – Recovery within 24–72 hours with supportive care alone
- Moderate bites – Deterioration begins in 6–12 hours without treatment
- Severe cases – Rapid decline leads to death within hours
- Snake bite survival depends on venom load, medical response speed, and individual health factors
Lethality rates prove early intervention matters most.
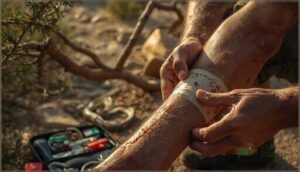
What First Aid Can Help if No Treatment is Available?
If you’re bitten in a remote area with no medical help nearby, certain first aid steps can slow venom spread and buy you critical time. However, you also need to know what actions make things worse—some traditional “remedies” can actually increase tissue damage or speed venom circulation.
Let’s break down what helps, what harms, and what’s pure myth.
Immediate Steps to Slow Venom Spread
If you’re bitten and help isn’t coming soon, your actions matter. Keep the bitten limb still and positioned at heart level—not elevated or dangling—to slow venom spread through your bloodstream. Remove rings, watches, or tight clothing near the wound before swelling kicks in. Most importantly, get someone calling for emergency care while you stay calm and minimize movement.
| Do This | Why It Helps | Timing |
|---|---|---|
| Keep limb at heart level | Slows venom circulation | Immediately |
| Remove jewelry/tight items | Prevents constriction from swelling | First 5 minutes |
| Stay still and calm | Reduces venous return | Until help arrives |
Actions to Avoid After a Bite
Skip old-school tactics that worsen rattlesnake bite outcomes. Don’t apply a tourniquet—it traps venom and damages tissue. Never cut the bite site or attempt venom sucking. Ice application causes further injury, and sedative use masks critical symptoms.
Most importantly, don’t handle the snake for identification. These misguided first aid moves increase harm from venomous snakes when you need treatment most.
Myths and Ineffective Remedies
You’ll hear plenty of bad advice about snake bite treatment—ignore it. Folk remedies and venom myths waste precious time when you need real medical care for venomous snakes.
- Tourniquet risks: Cutting off circulation traps venom and destroys tissue
- Suction methods: Attempting to extract venom introduces infection without removing toxins
- Ice treatment: Freezing tissue worsens damage instead of slowing spread
- Plant extracts and internet cures: Unproven home remedies delay lifesaving antivenom and first aid
Can First Aid Alone Save You?
First aid helps, but it won’t replace what antivenom does. Think of it like bailing water from a sinking boat—you’re buying time, not fixing the hole.
Here’s what first aid can and can’t do when you’re facing rattlesnake venom without medical treatment.
Limitations of First Aid Without Antivenom
First aid can’t neutralize venom or replace antivenom for definitive recovery. Techniques like compression or incision lack evidence of benefit and may cause harm or infection. While slowing venom spread might delay systemic effects, it won’t reliably prevent them.
Transport to medical facilities remains critical—delays reduce first aid effectiveness. Without antivenom, long-term survival depends on organ resilience and hospital supportive care.
Temporary Measures Versus Definitive Treatment
There’s a reason emergency response teams prioritize antivenom over first aid alone. Temporary measures like immobilization can’t achieve venom neutralization—only medical intervention delivers that. While keeping the bite area still might buy you minutes, it won’t stop tissue destruction or organ damage. Here’s what separates stopgaps from survival:
- First aid slows venom spread temporarily but doesn’t reverse damage
- Antivenom efficacy depends on early administration at medical facilities
- Treatment outcomes improve dramatically with professional care versus field measures
- Medical attention provides monitoring for respiratory or cardiac complications
- Definitive treatment tackles venomous snakes’ systemic effects that first aid can’t touch
Every minute without proper medical intervention raises your risk of irreversible harm after a rattlesnake bite.
When First Aid May Prolong Survival
In remote wilderness scenarios where medical help is hours away, basic first aid becomes your best bet for buying critical time. Proper limb immobilization and staying calm can reduce venom effects by 30-40% during those vital first hours.
Here’s how wilderness first aid impacts survival rates:
| First Aid Tips | Impact on Bite Symptoms |
|---|---|
| Keep bite below heart level | Slows systemic venom spread |
| Remove jewelry immediately | Prevents circulation loss from swelling |
| Immobilize affected limb | Reduces venom absorption rate |
| Stay calm, move minimally | Lowers heart rate and venom circulation |
These venomous snake bites demand emergency response—but smart snake bite treatment in the field can stretch your survival window until help arrives.
What Are The Chances of Permanent Injury or Disability?
Even if you survive a rattlesnake bite without treatment, the battle isn’t over. Your body may carry lasting damage that affects your quality of life for months or even years. Let’s look at what permanent injuries and disabilities you might face.
Common Long-Term Consequences
Beyond the immediate danger, rattlesnake bite survivors face lasting damage even with medical attention. Studies show about 37% develop chronic kidney problems or renal failure within a year. Local tissue necrosis affects roughly 40% of upper extremity bites, while neuromuscular damage can persist for months.
Psychological trauma hits hard too—PTSD rates climb to 43% in some groups, and depression affects over half of survivors.
Risk of Limb Loss or Chronic Pain
Without treatment, your risk of losing a limb or dealing with chronic pain climbs sharply. Up to 25 percent of untreated rattlesnake bite victims develop persistent pain that haunts them long after the fangs pulled away.
Tissue death at the bite site can trigger contractures and nerve damage—problems that chronic pain management and limb salvage techniques may not fully reverse once the damage sets in.
Psychological Impact After Surviving
Surviving a rattlesnake bite doesn’t mean the battle ends when your wounds close. Emotional trauma runs deep—up to 79 percent of victims report PTSD symptoms. You might face:
- Flashbacks and hyperarousal months after the bite
- Depression in over half of survivors
- Anxiety disorders that disrupt daily life
- Somatic complaints like unexplained pain
- Social stigma if disability follows
Emergency medical response matters for your mind, not just your body.
Are There Natural Remedies or Home Treatments?
When you’re bitten by a rattlesnake, you might hear advice about natural remedies or home treatments from well-meaning sources. The reality is that none of these methods work, and some can make things worse.
Here’s what you need to know about unproven treatments and what experts actually recommend.
Dangers of Relying on Unproven Methods
Chasing false cures can cost you your life. Medical misconceptions about rattlesnake bite treatment are common, and unproven remedies often delay the care that actually saves limbs and lives.
Electric shocks, tourniquet application, cutting the wound, or herbal pastes won’t neutralize venom—they’ll waste critical time while toxins spread. Studies show treatment delays from these venom myths directly increase your risk of severe complications and death.
Common Myths About Snakebite Cures
You’ve probably heard someone swear that sucking out venom or applying a tourniquet will save you—but these old-school “cures” do more harm than good. Here are the most dangerous snake oil remedies still circulating:
- Sucking venom from the bite – ineffective and risks mouth contamination
- Cutting the wound open – causes tissue damage without removing rattlesnake venom
- Ice packs or alcohol – worsen tissue injury and delay proper first aid
Expert Recommendations
Seek emergent medical evaluation after any rattlesnake bite—period. Rapid transport to a facility equipped for antivenom therapy and emergency response offers your best shot at survival.
Medical guidance is clear: Treatment protocols emphasize evidence-based care, not folklore. Time matters in venomous snake encounters; delays increase systemic toxicity risk.
Don’t gamble with snake bite survival when definitive emergency medical response and venom research support antivenom as the benchmark treatment.
Why is Immediate Medical Care Critical?
When a rattlesnake bites you, the clock starts ticking. The difference between getting to a hospital and staying put can literally mean the difference between walking away whole or facing serious complications.
Let’s break down exactly why professional medical care isn’t optional—it’s your best shot at survival.
Role of Antivenom in Survival
Antivenom is your best shot at walking away from a rattlesnake bite without lasting damage. This medical intervention works by neutralizing venom in your bloodstream, stopping tissue destruction and preventing life-threatening complications.
Quick emergency response matters—getting antivenom within hours dramatically improves snakebite outcomes. The right antivenom dosage, determined by venom severity and species, can mean the difference between recovery and permanent disability after venomous snake bites.
Hospital Supportive Care and Monitoring
Hospital emergency care goes far beyond just giving you antivenom. Medical monitoring starts the moment you arrive—continuous checks of your heart, breathing, and blood pressure catch complications early.
Emergency stabilization includes IV fluids, pain management, and serial lab work every few hours. If things get dicey, intensive care with ventilator support or blood products becomes necessary.
Patient observation continues for 18–24 hours minimum, ensuring venom management stays on track.
Outcomes With and Without Professional Treatment
The contrast is stark: with professional medical treatment, rattlesnake bite mortality rates drop below 1 percent, while untreated cases historically showed 5–25 percent fatality.
With professional medical treatment, rattlesnake bite mortality drops below 1 percent—untreated cases historically killed 5 to 25 percent of victims
Treatment outcomes with antivenom include:
- Survival odds exceeding 99 percent in modern hospitals
- Normalized blood clotting within days
- Reduced tissue damage and disability risk
- Faster recovery processes and pain resolution
- Prevention of respiratory failure and organ damage
Medical intervention makes the difference between death and walking away whole.
Frequently Asked Questions (FAQs)
How long does it take for rattlesnake venom to kill?
Fatal timeframe varies widely. Most untreated rattlesnake bite deaths occur over two to three days from organ failure, though severe envenomation can kill within six to 48 hours depending on venom potency and bite severity.
Can sucking out the venom from a bite help?
Cutting open the bite wound and trying to suck out venom seems helpful—but creates two problems instead of one. Studies show suction removes less than 04 percent of rattlesnake venom.
Are baby rattlesnakes more dangerous than adult ones?
No. Adult rattlesnakes pose greater danger to humans than babies. Larger snakes inject far more venom per bite despite slightly lower venom potency in juveniles, resulting in more severe rattlesnake bite complications requiring higher antivenom doses.
What should you do if bitten while hiking alone?
Ironic, isn’t it? You chose solo wilderness first aid, and snakebite protocol matters most now.
Move away calmly, call emergency response, keep the limb still, and walk slowly toward remote rescue—snakebite survival strategies demand controlled evacuation.
Can rattlesnake antivenin cause allergic reactions in some people?
Yes, rattlesnake antivenom can trigger allergic reactions in some patients. Hypersensitivity responses range from mild rash to severe anaphylaxis. Documented allergic reaction rates vary, but most antivenin side effects remain manageable with prompt medical intervention.
How long can you survive without antivenom treatment?
Without antivenom, your survival window generally spans 48 to 72 hours in severe envenomation cases. Venom effects begin within minutes, but life-threatening complications—respiratory failure, shock, organ damage—usually develop over hours, not instantly.
What percentage of rattlesnake bites are fatal?
The mortality rate sits refreshingly low at roughly 14 percent when you receive care—about 1 death per 736 rattlesnake bites. Survival odds climb even higher with prompt antivenom and modern medical support.
Do all rattlesnake bites inject venom?
No—about 20 to 25 percent of rattlesnake bites are “dry,” delivering no venom at all.
Rattlesnakes can meter venom deliberately, sometimes choosing defensive warning strikes that conserve their metabolically expensive venom for hunting.
How quickly does rattlesnake venom spread?
Rattlesnake venom hits your bloodstream fast—within minutes through lymphatic spread—but full systemic effects unfold over hours. Venom bioavailability peaks under 30 minutes, yet tissue depots release toxins for days after the bite.
Can children survive rattlesnake bites better?
No. Children actually face higher risk from rattlesnake bites. Their smaller body mass means venom concentrates faster, requiring urgent pediatric venom treatment.
Youth treatment protocols demand immediate first aid procedures and specialized rattlesnake bite treatment to prevent severe complications.
Conclusion
Hope for the best, but prepare for the worst—that’s the mindset you need with rattlesnake bites. While you can survive a rattlesnake bite without treatment, the odds aren’t in your favor.
Venom doesn’t negotiate with luck or willpower. Antivenom exists for a reason: it works when your body can’t fight back fast enough.
Skip the gamble. Get to a hospital, protect your limbs and organs, and walk away whole instead of wondering what you could’ve saved.