This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.

You’ll notice discolored scales, raised patches, or areas where scales separate from underlying tissue.
These infections often start from poor husbandry—excessive moisture, wrong temperatures, or dirty enclosures create perfect breeding grounds for harmful microorganisms.
What begins as simple irritation can quickly escalate to deep, painful ulcers that threaten your snake’s life.
Blister disease, caused by prolonged dampness, represents one common pathway from minor skin issues to serious systemic infection.
Early recognition matters because untreated infections spread rapidly and can lead to sepsis.
Understanding the warning signs and treatment protocols can mean the difference between a quick recovery and permanent damage.
Table Of Contents
- Key Takeaways
- Common Causes of Snake Skin Infections
- Recognizing Symptoms of Snake Skin Infections
- Blister Disease in Snakes: Causes and Progression
- Diagnosing Snake Skin Infections and Ulcerations
- Treatment Options for Snake Skin Infections
- Preventing Snake Skin Infections and Ulcerations
- Managing Chronic Skin Conditions in Snakes
- Zoonotic Concerns With Snake Skin Infections
- Recovery and Prognosis for Infected Snakes
- Frequently Asked Questions (FAQs)
- What does a skin infection look like on a snake?
- What does snake skin rot look like?
- What is the early stage of snake blister disease?
- What does snake fungal disease look like?
- What are the symptoms of infectious stomatitis in reptiles?
- What is Paget’s disease in reptiles?
- Can snake skin infections spread to other pets?
- Are certain snake species more prone to skin infections?
- How often should I inspect my snake for skin issues?
- Can snake skin infections spread between different species?
- Conclusion
Key Takeaways
- Watch for early warning signs – You’ll spot snake skin infections through scale discoloration, raised rough patches, blisters, and behavioral changes, such as excessive rubbing or lethargy, before they become life-threatening.
- Environmental factors cause most infections – Poor husbandry, including excessive moisture, wrong temperatures, dirty enclosures, and inadequate ventilation, create perfect breeding grounds for bacteria and fungi that attack your snake’s skin.
- Quick veterinary intervention prevents complications – Don’t wait when you see symptoms; untreated skin infections rapidly progress from minor irritation to deep ulcers and potentially fatal sepsis within days.
- Prevention beats treatment every time – You’ll avoid most skin infections by maintaining proper humidity levels, consistent temperatures, clean substrates, and regular enclosure cleaning, rather than dealing with expensive treatments later.
Common Causes of Snake Skin Infections
Snake skin infections stem from multiple sources that can quickly compromise your pet’s health.
Understanding these common causes helps you recognize early warning signs and take prompt action to prevent serious complications.
This knowledge is crucial for preventing serious health issues in your pet.
Bacterial Infections in Snakes
Bacterial Causes lurk everywhere in your snake’s world. Poor Snake Hygiene creates perfect conditions for opportunistic bacteria to invade compromised skin.
Stress, dirty enclosures, and improper temperatures weaken your reptile’s immune defenses. These infections cause Scale Damage through inflammation and tissue breakdown.
Infection Control starts with maintaining clean habitats and proper husbandry. When bacterial infections strike, prompt veterinary care and appropriate Antibiotic Use can prevent progression to serious ulcerated skin conditions.
Fungal Infections Affecting Snake Skin
While bacterial culprits attack through wounds, fungal infections sneak in through environmental exposure.
These microscopic invaders thrive in damp conditions, making proper humidity control essential for prevention.
Snake fungal disease affects reptiles nationwide, with specific pathogens causing distinct symptoms:
- Fungal spores colonize damaged scales, creating circular skin lesions
- Scale fungus produces crusty, discolored patches requiring mycological tests for identification
- Dermatitis treatment involves antifungal medications targeting specific fungal strains
Ophidiomyces ophiodiicola represents the most studied pathogen, causing ulcerated skin and deep skin ulcers.
This snake skin infection spreads through contaminated substrates, making quarantine protocols essential for preventing transmission between animals.
Viral Infections Leading to Skin Issues
Viral infections strike snake skin through several pathways.
You’ll encounter snake pox, herpesvirus, and iridovirus as primary culprits.
These pathogens create distinctive skin lesions including pustules, blisters, and scaly patches.
Herpes symptoms often manifest as facial swelling and mouth ulcers.
Iridovirus effects include systemic weakness alongside dermal changes.
Pox outbreaks produce characteristic raised bumps across scales.
High viral loads compromise your snake’s immune system, making secondary infections likely.
These reptile diseases disrupt normal shedding cycles and create entry points for bacterial complications.
They can lead to systemic weakness, dermal changes, and secondary infections that further threaten the snake’s health.
Parasitic Infestations Causing Dermal Problems
Tiny troublemakers like dermal mites and ticks create serious problems for your snake’s skin.
These parasitic infestations cause intense itching, leading to excessive rubbing that produces skin lesions and potential ulcerated skin areas.
Mite infestations spread rapidly between reptiles, while tick borne diseases pose additional health risks.
You’ll notice small moving dots, unusual scratching behavior, or irritated patches on your snake’s scales.
Effective parasite control requires immediate veterinary intervention and thorough enclosure cleaning to prevent reinfestations and subsequent reptile skin diseases.
This approach is crucial for maintaining the health and well-being of your snake, and it should be taken seriously to avoid any further complications, including the risk of tick borne diseases.
Environmental Factors Contributing to Skin Infections
Poor environmental conditions create the perfect storm for reptile skin infections. Inadequate humidity control and temperature fluctuations stress your snake’s immune system, while dirty enclosures harbor dangerous bacteria.
Your snake’s home environment isn’t just comfort—it’s their first line of defense against infection.
Here’s what puts your snake at risk:
- Stagnant water breeding harmful microorganisms
- Poor air circulation trapping moisture and pathogens
- Substrate contamination from waste buildup
- Inconsistent heating creating bacterial growth zones
These environmental factors directly contribute to bacterial infections and ulcerated skin development, which can be exacerbated by inadequate care and poor husbandry practices, ultimately leading to serious health issues for your snake.
Recognizing Symptoms of Snake Skin Infections
Identifying snake skin infections early helps you provide prompt treatment and prevent serious complications. You’ll notice several key warning signs that indicate your snake needs immediate veterinary attention.
Visual Signs of Infection on Snake Scales
When examining your snake, watch for scale discoloration – red patches or dark spots signal trouble.
Skin lesions and blister formation appear as raised bumps or fluid-filled sacs.
Notice scale roughness where smooth scales become textured or raised.
Ulcer signs include open wounds with exposed tissue underneath.
Missing scales create bare patches on the skin.
These visual markers indicate bacterial infection or other pathogens affecting your snake’s health.
Changes in Skin Texture and Appearance
When examining your snake’s skin, texture changes often reveal infection before other symptoms appear.
Healthy snakes display smooth scales with consistent patterns, but infections disrupt this normal appearance.
Watch for these key texture changes:
- Scale discoloration ranging from red patches to dark spots
- Skin lesions with raised or rough edges indicating damage
- Pattern alterations where natural markings become distorted
- Color shifts showing unusual brightness or dullness in affected areas
These texture changes signal that infected skin needs immediate attention.
Ulcerated skin develops when infections progress untreated, creating open wounds that compromise your snake’s health and comfort.
Behavioral Changes Indicating Skin Discomfort
When your snake feels discomfort from skin infection, you’ll notice clear behavioral changes.
Increased lethargy signs and irritability factors become apparent as infected snakes grow restless.
Rubbing behavior against cage items indicates itching from ulcerated skin.
Watch for hiding more frequently, refusing meals, and general agitation.
These behavioral changes signal your snake’s distress from skin discomfort and require immediate attention.
Shedding Abnormalities Associated With Infections
Shedding Issues become obvious when snake skin infection strikes your pet.
Watch for Abnormal Molting patterns like incomplete sheds or retained skin patches.
Scale Damage and Skin Lesions disrupt normal shedding cycles, creating Infection Signs you can’t miss.
Shedding abnormalities often signal snake fungal disease or bacterial problems affecting infected skin.
These ulcerated skin areas prevent proper molting, leaving stuck skin that worsens the condition.
Presence of Discharge or Odor From Affected Areas
Your snake’s discharge signs tell a clear story.
Look for yellow, green, or bloody fluid seeping from skin lesions – these indicate bacterial infection or wound infection.
Foul odors signal serious infection sources requiring immediate attention.
Infected skin produces thick, sticky discharge that blocks natural wound healing.
Ulcerated skin often weeps constantly.
Document discharge color, consistency, and smell when contacting your veterinarian for proper snake skin infection treatment.
Blister Disease in Snakes: Causes and Progression
Blister disease develops when you keep your snake in consistently damp conditions, creating an ideal environment for bacterial growth on the skin.
This condition starts with small, fluid-filled blisters that can quickly progress to painful, open wounds if you don’t address the underlying husbandry problems.
Factors Leading to Blister Disease Development
Several environmental factors work together to create the perfect storm for blister disease in your snake. Excessive humidity ranks as the top culprit, especially when levels stay above your species’ requirements for 24-48 hours.
Your snake’s immune system weakens under chronic stress from temperature fluctuations, poor hygiene, and contaminated substrates. Understanding these triggers helps you recognize warning signs before blisters develop.
- Wet bedding and inadequate ventilation create bacterial breeding grounds
- Rough substrates cause skin trauma that invites opportunistic infections
- Immunosuppression from improper husbandry practices reduces natural resistance
Environmental stress doesn’t just affect comfort—it directly impacts your snake’s ability to fight off bacterial dermatitis and fungal pathogens like Ophidiomyces ophiodiicola, turning minor issues into serious ulcerated skin problems. Researchers study snake fungal disease to better understand its effects on snake populations.
Early Stages of Blister Formation
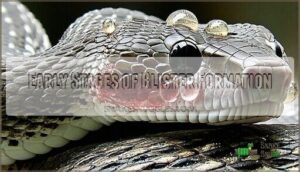
Blister formation starts subtly but progresses predictably.
You’ll notice redness first as inflammation begins beneath your snake’s scales. Swelling follows as fluid accumulates, creating raised areas.
Soon, actual blisters form when skin lifts, creating characteristic bubbles filled with fluid. The affected area often darkens, and individual scales may appear raised or separated.
These infection signs indicate scale damage requiring immediate attention, as they can lead to more serious issues if not addressed promptly, including potential long-term inflammation.
Progression of Blisters to Ulcerated Skin
Rupturing blisters expose raw tissue beneath, creating open wounds.
These areas quickly expand and merge, forming patches of ulcerated skin.
Skin ulceration occurs when protective scales separate from underlying tissue.
Infection stages progress rapidly without treatment.
Wound healing becomes compromised as bacteria colonize exposed areas.
Blister disease symptoms worsen as tissue damage spreads across your snake’s body.
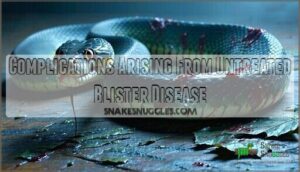
Complications Arising From Untreated Blister Disease
When blister disease goes untreated, your snake faces serious health risks.
The infection can quickly spiral into life-threatening complications that affect multiple body systems.
Key complications include:
- Septicemia Risk – Bacteria enter the bloodstream, causing systemic infection and potential organ failure
- Skin Ulceration – Blisters rupture and create deep wounds that won’t heal properly without treatment
- Infection Spread – The bacterial dermatitis can move to bones, joints, and internal organs
Immune Suppression weakens your snake’s natural defenses, making Organ Damage more likely.
Early intervention prevents these devastating outcomes in reptile dermatology cases.
Differences Between Blister Disease and Other Skin Conditions
Identifying bacterial dermatitis versus blister disease requires careful observation.
Blister disease creates fluid-filled bumps that rupture into skin ulcers, while fungal infections produce dry, scaly patches.
Snake lesions from viral causes spread widely across the body.
Parasitic mites leave tiny red spots or tracks.
Environmental burns create uniform damaged areas.
Each snake skin infection has distinct patterns – blister disease shows localized fluid-filled sacs, dermatitis causes vary by pathogen type.
Diagnosing Snake Skin Infections and Ulcerations
When you suspect your snake has a skin infection, accurate diagnosis requires systematic evaluation by a qualified reptile veterinarian.
Proper diagnostic techniques combine visual examination, laboratory testing, and sometimes imaging to identify the specific pathogen and determine appropriate treatment.
Physical Examination Techniques for Infected Snakes
When examining your snake for infections, you’ll need systematic assessment techniques.
Check these key areas during your physical examination:
- Scale Inspection – Look for discoloration, raised edges, or unusual texture changes
- Skin Palpation – Feel gently for lumps, swelling, or temperature variations
- Mouth Examination – Check inside for redness, swelling, or discharge
- Thermal Imaging – Monitor body temperature patterns for infection indicators
- Ultrasonic Scanning – Detect deeper tissue involvement in severe cases
This thorough approach helps identify snake skin infection and ulcerated skin early.
Laboratory Tests for Identifying Pathogens
Once your vet completes the physical exam, they’ll typically run laboratory tests to identify specific pathogens.
Culture methods grow bacteria and fungi from skin samples, while microscopy tests reveal parasites and cellular changes. PCR analysis detects viral DNA, and serology tests identify antibodies.
Cytology examines cell samples under magnification. These laboratory culture techniques help distinguish gram-negative bacteria from other causes, ensuring targeted treatment for bacterial infections.
The diagnosis of reptile diseases often involves understanding viral disease causes to provide effective treatment.
Imaging Methods to Assess Infection Severity
Modern imaging methods reveal infection severity beneath your snake’s scales.
Advanced diagnostics help veterinarians assess damage and plan effective ulcer treatment strategies.
- X-ray imaging detects bone involvement and deep abscesses
- Ultrasound scans locate fluid pockets and tissue damage
- CT scans map infection extent with detailed cross-sections
These radiography techniques guide wound care decisions for ideal healing outcomes.
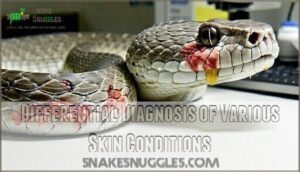
Differential Diagnosis of Various Skin Conditions
When multiple skin conditions look identical, your vet plays detective.
Skin lesions from bacterial dermatitis, fungal infections, and viral causes often appear similar.
Through cytology, histology, and culture tests, they distinguish between dermatitis types and infection stages.
Proper differential diagnosis prevents misidentifying scale disorders, ensuring targeted snake skin infection treatment for ideal wound healing of ulcerated skin.
Importance of Veterinary Expertise in Diagnosis
Professional veterinary expertise transforms snake health outcomes when skin infection strikes your scaly companion. You can’t replace years of specialized training with internet searches.
Veterinary professionals offer three key advantages:
- Diagnostic tools like microscopy and bacterial cultures reveal hidden pathogens
- Medical imaging detects deeper tissue involvement in ulcerated skin cases
- Expert opinion distinguishes bacterial dermatitis from similar conditions
Their treatment plans target specific causes rather than guessing games, ensuring your snake gets proper care.
Treatment Options for Snake Skin Infections
When your snake develops skin infections or ulcerations, prompt treatment prevents complications and promotes faster healing.
You’ll need to work with a reptile veterinarian to identify the specific pathogen and choose the most effective treatment approach.
Topical Medications for Skin Infections
Topical treatments offer direct relief for infected snake skin.
Antiseptic solutions clean wounds while antibiotic cream fights bacterial infections.
Antifungal sprays target fungal issues, and specialized skin ointments promote healing.
Proper medication application involves gentle cleaning first, then applying treatments as your vet directs.
Wound care products help damaged scales recover faster than systemic treatments alone.
Effective skin infection management often relies on using antibiotic products to prevent further complications.
Systemic Antibiotic Therapy for Bacterial Infections
When bacterial strains invade your snake’s skin, systemic antibiotics become essential weapons in infection control.
Your vet will select targeted antibiotic therapy based on culture results to combat antibiotic resistance.
Common choices include ceftazidime, enrofloxacin, and amikacin for reptile bacterial infections.
Proper dose administration and therapy duration guarantee complete eradication of snake skin infection while preventing treatment-resistant bacterial strains, which is crucial for effective infection control.
Antifungal Treatments for Fungal Skin Issues
When fungal infections strike your snake’s skin, antifungal treatments become essential weapons in your care arsenal.
These medications target stubborn fungal dermatology issues that topical treatments alone can’t handle.
Here’s your treatment approach:
- Antifungal cream applied directly to affected scales twice daily
- Fungal medications prescribed by your vet for severe infections
- Topical treatments combined with environmental humidity control
- Skin fungus monitoring to track healing progress over weeks
Remember, consistent application defeats these persistent invaders.
Supportive Care for Infected Snakes
Thorough care extends beyond medication when treating snake skin infection.
Proper hydration management guarantees adequate fluid intake while maintaining species-appropriate humidity levels.
Nutrition therapy strengthens immune function through high-quality prey items delivered on schedule.
Environmental adjustments include optimizing temperature gradients and eliminating stressors that compromise healing.
Regular wound cleaning prevents secondary skin bacteria colonization in infected wounds.
Minimize handling to reduce stress and promote natural wound healing.
Pain relief may be necessary for severe cases affecting mobility or feeding behavior.
Effective snake wound care involves understanding proper wound care products to support the healing process.
Surgical Interventions for Severe Ulcerations
When supportive care isn’t enough, surgical interventions save lives.
Veterinarians perform ulcer debridement to remove dead tissue from ulcerative dermatitis lesions.
Wound closure techniques repair damaged areas, while tissue grafting and skin reconstruction restore severely affected regions.
These surgical repair procedures prevent septicemic conditions from developing.
Debridement of infected snake skin infection sites promotes healing and stops complications before they become life-threatening emergencies.
Preventing Snake Skin Infections and Ulcerations
Prevention is your most powerful weapon against snake skin infections and ulcerations.
You can protect your snake’s health by maintaining proper husbandry practices, monitoring environmental conditions, and catching problems early through regular check-ups.
Proper Husbandry Practices for Snake Health
Proper husbandry forms the foundation for preventing snake skin infection and maintaining ideal reptile skin conditions.
Your commitment to excellent Snake Handling and consistent Enclosure Cleaning directly impacts skin infection prevention. Properly designed snake enclosure systems are vital for maintaining a healthy environment.
Focus on three critical husbandry elements:
- Feeding Schedule: Provide appropriately-sized, pre-killed prey items on species-specific intervals
- Water Quality: Supply fresh, clean water weekly with immediate substrate removal after soiling
- Record Keeping: Document feeding responses, weight changes, and behavioral patterns for early problem detection
Maintaining Optimal Environmental Conditions
Your snake’s environment directly impacts skin health through multiple factors.
Temperature control should maintain species-specific ranges – too hot causes burns, too cold weakens immunity.
Humidity management prevents excessive moisture that breeds bacteria while avoiding dryness that cracks scales.
Enclosure cleaning removes pathogens and waste buildup.
Air quality monitoring guarantees proper ventilation prevents stagnant conditions.
Water quality management provides clean drinking sources.
Lighting optimization supports natural rhythms and vitamin synthesis.
These optimal environmental conditions work together, preventing environmental stressors that compromise your snake’s immune system and create infection opportunities.
Regular Health Monitoring and Veterinary Check-ups
Daily Health Checks become your frontline defense against snake skin infection and skin conditions. Watch for scale discoloration, texture changes, or behavioral shifts that signal trouble brewing.
- Examine scales weekly for redness, swelling, or unusual bumps indicating developing skin infection
- Schedule veterinary attention every 6-12 months for professional wellness assessments and Preventive Measures
- Document changes in appetite, shedding patterns, or activity levels through consistent Monitoring Systems
Regular health monitoring paired with professional Veterinary Care catches problems before they escalate into serious Snake Wellness concerns.
Proper skin health management is essential for preventing snake skin infections and promoting overall snake well-being.
Quarantine Procedures for New or Sick Snakes
When building your collection grows, isolation techniques become your shield against skin infections spreading throughout your facility. New arrivals or sick snakes need immediate separation from healthy animals.
Establish effective quarantine protocols by setting up a designated space with:
- Clean, disinfected enclosure with minimal décor
- Disposable substrate for easy replacement
- Separate handling tools and feeding equipment
- Dedicated cleaning supplies for quarantine area only
Quarantine duration should extend 30-90 days for new snakes, allowing time to detect latent infections. During this period, maintain strict biosecurity measures – wash hands thoroughly between animals and change clothes when moving between quarantine and main collection areas.
Snake acclimation occurs gradually as you monitor for symptoms like scale discoloration, lethargy, or abnormal shedding patterns. Proper sanitation methods require daily spot-cleaning and weekly deep disinfection of all surfaces to prevent snake skin infection transmission.
Proper Handling Techniques to Minimize Skin Damage
When supporting your snake’s body weight, distribute pressure across multiple contact points to prevent scale compression.
Use gentle handling techniques with clean, dry hands to avoid transferring bacteria that cause snake skin infection.
Support the snake’s midsection and rear third, never gripping tightly.
Conduct brief skin inspection during handling sessions, checking for discoloration or raised scales.
Limit snake handling to 10-15 minutes to reduce stress-induced skin damage.
Proper snake support and injury prevention through careful scale care protect against reptile bites and maintain snake skin hygiene.
Managing Chronic Skin Conditions in Snakes
When you’re caring for a snake with chronic skin conditions, you’ll need to shift from treating acute infections to managing ongoing health challenges.
This means creating specialized care protocols that address both the underlying causes and prevent future flare-ups while supporting your snake’s long-term wellbeing.
Long-term Care for Recurrent Infections
Recurrent infections demand a systematic approach to Infection Management. You’ll become your snake’s personal health detective, tracking patterns and triggers.
Long Term Healing requires these five strategies:
- Document infection patterns – note timing, severity, and environmental factors
- Establish baseline husbandry parameters – temperature, humidity, substrate type
- Implement prophylactic treatments – regular antiseptic washes during high-risk periods
- Monitor stress indicators – feeding response, activity levels, defensive behaviors
- Schedule preventive veterinary assessments – quarterly check-ups for Chronic Care patients
Understanding skin infection treatment is essential for effective management. Skin Rehabilitation becomes easier when you identify your snake’s specific triggers and create personalized prevention protocols.
Dietary Considerations for Skin Health
Nutrient balance directly impacts your snake’s ability to fight off snake skin infections.
Feed prey items rich in vitamin A – nutritional deficiencies weaken immune systems and slow healing.
Mineral intake from whole prey provides zinc and selenium for healthy scales.
Avoid dietary fiber supplements unless prescribed.
Quality reptile nutrition beats quantity every time.
Skin supplements may help during recovery, but proper vitamin requirements through natural prey remain your best defense against recurring skin health issues.
Adaptation of Enclosure for Affected Snakes
When your snake’s skin needs TLC, their home becomes part of the treatment.
Enclosure Cleaning keeps bacteria at bay while Humidity Control maintains proper moisture levels for healing.
Adjust Temperature Management to support immune function and choose softer Substrate Selection that won’t irritate wounds.
Lighting Adjustment with appropriate UVB helps recovery.
Transform your snake’s space into a healing sanctuary where skin damage can mend through proper reptile husbandry and thoughtful enclosure design.
Monitoring and Preventing Secondary Infections
Recovery requires continuous vigilance to prevent secondary infections from derailing your snake’s healing journey.
Monitor wound sites daily for new inflammation or discharge that signals bacterial dermatitis complications.
Effective infection prevention demands:
- Daily wound care inspections checking for redness, swelling, or unusual odor
- Strict infection control protocols maintaining sterile handling and clean enclosure surfaces
- Proactive management strategies adjusting humidity levels and implementing preventive skin monitoring routines
Secondary prevention protects your snake’s compromised immune system during recovery.
Rehabilitation Strategies for Severely Affected Snakes
Rehabilitation techniques for snakes with ulcerative dermatitis require patience and systematic care.
Start with nutritional support through easily digestible prey items to boost immune function. Maintain strict snake wound care protocols using antiseptic solutions for wound healing.
Environmental enrichment includes temperature gradients and humidity control. Physical therapy involves gentle handling to prevent muscle atrophy.
In severe cases, skin grafts may be necessary. Monitor snake skin recovery closely, adjusting rehabilitation techniques based on healing progress.
This thorough approach guarantees successful snake skin infection treatment and long-term health.
Zoonotic Concerns With Snake Skin Infections
While snake skin infections rarely spread to humans, you’ll want to take precautions when handling infected reptiles.
Certain bacteria like Salmonella can transmit from snakes to people, potentially causing gastrointestinal illness in handlers who don’t follow proper hygiene protocols.
Potentially Transmissible Pathogens to Humans
When handling infected snakes, you’re potentially exposed to various pathogens that pose zoonotic risks.
These transmissible pathogens can cause human infections through direct contact with ulcerated skin.
Key pathogens include:
- Salmonella – Found in 56% of snakes, causing gastrointestinal illness
- Mycobacterium – Leads to pulmonary and skin infections in humans
- Pseudomonas aeruginosa – Causes opportunistic infections including sepsis
- Proteus vulgaris – Results in urinary tract infections
- Candida species – Causes superficial or invasive fungal infections.
Human infections occur through direct contact with contaminated surfaces or snake secretions.
Safety Precautions When Handling Infected Snakes
You need proper protection when handling infected snakes to prevent disease transmission.
Always wear disposable nitrile gloves and long-sleeved clothing to avoid direct skin contact. Use gentle snake restraint techniques to minimize stress while maintaining your safety.
| Safety Measure | Protection Level | Application Method |
|---|---|---|
| Nitrile gloves | High barrier protection | Replace between animals |
| Long sleeves/pants | Physical skin barrier | Cover all exposed skin |
| Minimal handling | Reduces exposure time | Essential tasks only |
Proper Sanitation and Hygiene Practices
Beyond safe handling, maintaining strict hygiene standards protects both you and your snake.
Effective sanitation methods require consistent application of cleaning protocols throughout your routine.
Essential sanitation practices include:
- Disinfection techniques – Use reptile-safe cleaners on all surfaces after contact
- Enclosure maintenance – Clean substrate, water bowls, and décor weekly minimum
- Personal hygiene practices – Wash hands thoroughly before and after snake interactions
These snake sanitation practices prevent cross-contamination and reduce infection spread.
Regular cleaning and maintenance also help prevent skin health issues that can lead to more severe problems if left unchecked.
Recognizing Symptoms of Zoonotic Infections
Human Risk associated with snake skin infection requires vigilant monitoring.
Watch for redness, swelling, or unusual warmth around bite sites or areas touched by infected reptiles.
Fever, lymph node enlargement, and red streaking indicate serious bacterial infections requiring immediate medical attention.
Skin ulcers developing after reptile contact suggest potential zoonotic transmission.
Disease Prevention starts with recognizing these warning signs early.
Most reptile zoonotic risks remain low, but Infection Control depends on prompt symptom recognition.
Public Health guidelines emphasize monitoring for 48-72 hours post-exposure to identify developing zoonotic concerns before complications arise, which is crucial for Disease Prevention and effective Infection Control to prevent serious bacterial infections, including those indicated by red streaking, and to address potential zoonotic transmission.
Importance of Personal Protective Equipment
Proper personal protective equipment protects you from snake zoonotic risks during antiseptic therapy.
Glove safety prevents direct contact with infected skin. Mask protocols and eye protection block airborne pathogens.
Hand sanitizers eliminate surface bacteria after handling. Biohazard suits offer maximum protection for severe snake skin infection cases.
Your safety gear isn’t optional—it’s your first line of defense.
Recovery and Prognosis for Infected Snakes
Your snake’s recovery depends on several key factors including the infection type, severity, and how quickly you begin treatment.
Most skin infections heal within 2-8 weeks with proper care, though severe ulcerations may take several months and could leave permanent scarring, which is influenced by the overall severity.
Factors Influencing Recovery From Skin Infections
Your snake’s recovery from skin infections depends on several key factors that work together like a well-oiled machine.
Core Recovery Factors:
- Nutrition Therapy – Well-fed snakes heal faster through proper protein intake
- Environmental Adjustments – Ideal temperature and humidity support wound healing
- Immune System strength – Natural defenses fight bacterial dermatitis effectively
- Recovery Timeframe – Early intervention speeds snake skin infection resolution
Timeline for Healing of Ulcerated Skin
Recovery time for ulcerated snake skin infection depends on multiple factors.
Minor wounds typically heal within two to four weeks with proper wound management. Deeper ulcerations may require six to twelve weeks for complete skin regeneration.
Healing stages progress from infection clearance to wound closure, then skin health restoration. Recovery time accelerates with prompt treatment and ideal healing assistance.
Quick Healing Slow Healing
Potential Long-term Effects on Snake Health
Chronic infection leaves permanent marks on your snake’s body and health.
Skin scarring from severe snake skin ulceration can restrict movement and growth.
Organ damage may occur when bacteria spread systemically, causing snake septicemia.
Immune suppression makes future infections more likely.
Some snakes experience stunted growth or behavioral changes that persist long after healing.
Monitoring for Relapses or Recurring Infections
Vigilant observation becomes your best defense against relapse prevention once initial treatment concludes. Weekly skin inspections help catch early warning signs before they escalate into serious snake skin infections.
Track these critical indicators for effective health monitoring:
- Scale discoloration or texture changes – New redness, swelling, or rough patches signal potential infection tracking needs
- Behavioral shifts – Increased rubbing, lethargy, or appetite loss may indicate recurring snake skin ulcer development
- Shedding irregularities – Incomplete or delayed sheds often precede skin regeneration problems
Document observations in a health log, noting dates and specific changes. This systematic approach supports post treatment care by establishing baseline patterns for your snake’s recovery. Contact your veterinarian immediately if suspicious symptoms appear – early intervention prevents minor issues from becoming major reptile skin infections requiring extensive snake infection prevention protocols.
Rehabilitation Techniques for Recovered Snakes
After monitoring your snake through recovery, proper rehabilitation techniques become your next focus. These methods guarantee complete healing and prevent future snake skin infections.
Post Infection Care starts with gradually adjusting your snake’s environment. Start with controlled temperatures and humidity levels that support skin regeneration. Recovery nutrition plays a key role – offer appropriately sized prey items to rebuild strength without overwhelming their system.
Rehabilitation methods include:
- Gentle handling sessions to reduce stress and monitor healing progress
- Environmental enrichment with clean hides and climbing opportunities
- Gradual exercise introduction through supervised exploration time
- Regular skin assessments to track snake skin healing and catch early signs of relapse
Snake rehabilitation requires patience as the snake recovery timeline varies by species and infection severity. Reptile wound management continues during this phase, with careful attention to any remaining sensitive areas. Some owners consider snake rehoming if long-term care needs exceed their capabilities, guaranteeing their pet receives appropriate specialized care.
Frequently Asked Questions (FAQs)
What does a skin infection look like on a snake?
Snake infections look absolutely horrific—you’ll spot discolored scales (red to dark patches), raised rough edges, blisters, ulcerated skin, discharge, and odor.
Affected snakes show lethargy, excessive rubbing, and abnormal shedding patterns requiring immediate veterinary care.
What does snake skin rot look like?
You’ll notice reddish-brown patches with raised, roughened scales that feel bumpy.
Blisters may form and rupture, exposing raw, ulcerated tissue underneath.
The affected areas often emit a foul odor and appear swollen or inflamed.
What is the early stage of snake blister disease?
Early blister disease in snakes shows red, swollen skin areas that develop into fluid-filled blisters.
You’ll notice inflammation and raised bumps before the blisters actually form, typically starting on the belly.
What does snake fungal disease look like?
You’ll spot facial swelling, raised nodules, and crusty ulcerations on your snake’s head and body. The fungus Ophidiomyces ophiodiicola creates distinctive lesions that differ from bacterial infections.
What are the symptoms of infectious stomatitis in reptiles?
You’ll notice mouth rot causes bloody spots, thick mucus, and pus in your snake’s mouth. The gums become red and swollen, making eating difficult and painful for your pet.
What is Paget’s disease in reptiles?
Looking for clarity on reptilian health conditions?
Paget’s disease isn’t a recognized condition in reptiles – you might be thinking of similar metabolic bone diseases or infections that affect reptilian skeletal systems and skin health, related to reptilian health.
Can snake skin infections spread to other pets?
Most snake skin infections don’t spread to other pets like cats or dogs.
However, some bacterial pathogens can cross species barriers.
You should isolate infected snakes and maintain strict hygiene when handling to prevent contamination.
Are certain snake species more prone to skin infections?
Yes, certain snake species are more susceptible to skin infections.
Ball pythons, boa constrictors, and corn snakes face higher risks due to their specific humidity requirements and stress sensitivity, making proper husbandry absolutely critical.
How often should I inspect my snake for skin issues?
Like a watchful guardian tending their precious charge, you’ll want to examine your snake weekly during routine maintenance.
Check scales for discoloration, roughness, or unusual patches while cleaning their enclosure.
This regular inspection helps catch early signs of dermatitis before serious complications develop.
Can snake skin infections spread between different species?
Cross-species transmission of snake skin infections is possible, especially with fungal pathogens like Ophidiomyces ophiodiicola.
You’ll need strict quarantine protocols and separate handling equipment to prevent spread between your different snake species.
Conclusion
Like a house’s foundation crack that spreads through walls when ignored, a small scale discoloration in your snake can quickly become a life-threatening infection.
Snake skin infection and ulcerated skin demand immediate attention and proper treatment. You’ve learned to recognize early warning signs, understand environmental triggers, and implement effective treatment protocols.
Quick action prevents minor issues from becoming serious health crises.
Proper husbandry creates the foundation for healthy skin, while regular monitoring catches problems early.
Your snake’s recovery depends on consistent care and professional veterinary guidance when needed.
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5095536/
- https://www.merckvetmanual.com/exotic-and-laboratory-animals/reptiles/bacterial-diseases-of-reptiles
- https://lbah.com/reptile/snake-skin-conditions/
- https://www.wildlifedemonstrations.com/post/scale-rot-how-to-identify-and-treat
- https://dep.nj.gov/njfw/wp-content/uploads/njfw/snake_fungal_disease.pdf