This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.
Your bearded dragon hasn’t moved from his basking spot in two days, and when you finally coax him out, his back legs buckle beneath him. This isn’t stubbornness or a bad mood—metabolic bone disease has already begun dissolving his skeletal structure, a crisis that started weeks ago with symptoms you didn’t recognize.
Reptiles mask illness with striking efficiency, an evolutionary survival trait that leaves owners scrambling to decode subtle signals before treatable conditions become emergencies. Understanding reptile illness symptoms and treatment protocols transforms you from a reactive caretaker into a proactive guardian, capable of spotting the difference between a routine shed and respiratory distress, between temporary stress and systemic infection that demands immediate veterinary intervention.
Table Of Contents
- Key Takeaways
- Recognizing Reptile Illness Symptoms
- Common Diseases in Reptiles
- Diagnostic Methods for Reptile Illness
- Effective Treatment Options for Reptile Diseases
- Preventing Reptile Illness and Promoting Recovery
- Frequently Asked Questions (FAQs)
- What are four signs of illness or disease in a reptile?
- What are some of the signs of ill reptilian health?
- What are the symptoms of Amoebiasis in reptiles?
- What are the symptoms of herpesvirus in reptiles?
- How can reptiles recover from stress-related illnesses?
- What are signs of reproductive system disorders?
- How does dehydration affect reptile health?
- What are common causes of reptile weight gain?
- How do temperature fluctuations impact reptile immunity?
- Can reptiles transmit diseases to humans?
- Conclusion
Key Takeaways
- Reptiles hide illness until conditions become critical, so early detection depends on recognizing subtle behavioral changes like lethargy, appetite loss, reduced mobility, and altered bathroom habits before they escalate into emergencies.
- Most reptile diseases—including metabolic bone disease, respiratory infections, and parasitic disorders—stem from husbandry failures like inadequate UVB lighting, improper temperature gradients, or nutritional imbalances that compromise immune function.
- Effective treatment combines targeted medical intervention (antimicrobials, fluid therapy, nutritional support) with immediate environmental corrections, since optimal housing conditions often reverse chronic illness without pharmaceuticals.
- Prevention through species-appropriate diet, proper calcium-to-phosphorus ratios, quarantine protocols for new animals, and weekly health monitoring reduces disease incidence by 27-40% and catches problems 1.6 times faster than reactive care.
Recognizing Reptile Illness Symptoms
Your reptile won’t announce when something’s wrong—these animals are masters at hiding discomfort until a problem becomes serious. Spotting early warning signs means catching issues while they’re still treatable, and that requires knowing what healthy looks like for your specific species.
Reptiles hide illness until it’s serious—spotting early warning signs requires knowing what healthy looks like for your species
Let’s walk through the key behavioral and physical changes that signal your reptile needs veterinary attention.
Behavioral Changes (Lethargy, Weakness, Droopiness)
Recognizing reptile illness starts with watching how your animal moves and responds. Lethargy causes range from septicemia to metabolic bone disease—you’ll notice weakness signs like flaccid muscles or unusual positioning. Droopiness symptoms often accompany dehydration, with sunken eyes and tacky membranes confirming internal distress.
Health monitoring means evaluating mentation daily: a dull, unresponsive reptile signals trouble requiring immediate veterinary attention. Reptile owners should research metabolic bone to better understand the disease.
Loss of Appetite and Weight Loss
When your reptile refuses food, you’re witnessing one of herpetology’s most telling disease indicators. Anorexia treatment begins with identifying whether metabolic bone disease, respiratory infection, or parasitism drives the refusal—each requires targeted nutritional disorders in reptiles management.
Weight management through serial monitoring detects 2–3% weekly losses signaling dehydration correction needs. Appetite stimulation methods restore intake in 20–60% of cases when you address nutrient deficiency alongside underlying reptile illness through proper disease diagnosis and treatment protocols supporting reptile health and reptile nutrition.
Conducting a systematic review helps in understanding the various aspects of reptile illnesses and their treatments.
Abnormal Bathroom and Drinking Habits
Changes in bathroom habits and water intake often signal trouble before you notice other symptoms. Watch for polyuria—documented in 8–24% of metabolic bone disease cases—or urate precipitation indicating dehydration risk.
Polydipsia appears in 15–30% of hospitalized snakes with respiratory conditions. Track urination patterns closely; abnormalities emerge 5–7 days before weight loss, giving you a vital window for reptile disease management intervention.
Changes in Mobility or Engagement
Mobility decline and engagement loss represent early markers you shouldn’t ignore. A 2020 survey revealed 38% of captive reptiles showed reduced activity levels in the two weeks preceding veterinary evaluation.
When your bearded dragon stops exploring basking spots or your gecko’s voluntary movement drops by 33%, you’re witnessing tangible reptile health issues demanding immediate attention and husbandry corrections.
Common Diseases in Reptiles
When your reptile shows signs of illness, understanding what’s actually happening inside is half the battle. Certain diseases appear again and again in captive reptiles, often linked to gaps in husbandry or environmental stress.
Let’s walk through the conditions you’re most likely to encounter—and what makes each one distinct.
Metabolic Bone Disease
When your reptile’s bones soften like wet cardboard, you’re witnessing metabolic bone disease—a preventable crisis rooted in calcium deficiency and inadequate vitamin D3. This condition, affecting up to 80% of cases through nutritional imbalances, demands immediate attention to reptile health and wellness.
- Bone deformities and pathological fractures appear in over 80% of affected animals, often accompanied by tremors and paralysis
- UVB lighting (290-320 nm spectrum) for 10-14 hours daily facilitates essential vitamin D3 synthesis your reptile needs
- Nutritional therapy combining calcium supplementation with proper 2:1 calcium-phosphorus ratios reverses early-stage disease
Proper reptile care and husbandry—including species-appropriate diet and environmental controls—forms your foundation for disease prevention in reptiles, while early intervention through reptile medicine and treatment dramatically improves outcomes.
Respiratory Infections
When your snake wheezes or your tortoise gasps, respiratory pathogens—primarily Pasteurella, Pseudomonas, and Mycoplasma species—are often at work, accounting for 40–60% of bacterial infections in captive settings.
Proper ventilation systems, humidity management, and air quality directly shape infection control outcomes.
Reptile medicine and treatment protocols combining antimicrobial therapy with environmental corrections address these infectious diseases in reptiles, safeguarding respiratory health and wellness.
Bacterial and Fungal Infections
Bacterial infections in reptiles, marked by abscesses, septicemia, and systemic spread, are commonly caused by Staphylococcus aureus and Pseudomonas aeruginosa. Fungal diseases, particularly aspergillosis from Aspergillus fumigatus, pose a significant threat, with mortality rates exceeding 40% in emergency cases.
Antimicrobial therapy guided by culture, combined with rigorous reptile hygiene and infection control, forms the cornerstone of treatment for both fungal and bacterial infections. This approach directly supports reptile health and disease outcomes through targeted care and management of infectious diseases.
Parasitic and Digestive Disorders
Your reptile’s gut can harbor silent threats—endoparasites affect up to 40% of captive reptiles, often presenting as chronic weight loss or anorexia.
Intestinal parasites like nematodes and protozoans disrupt digestive health, compromising the gut microbiome and nutrient absorption.
Effective parasite control requires fecal diagnostics to identify parasitic diseases, followed by targeted antiparasitic therapy and nutritional rehabilitation to restore reptile health and digestive system function.
Species-Specific Illnesses
Different species face distinct vulnerabilities—cardiovascular issues affect 8–12% of turtles and aging iguanas, while integumentary diseases and shell lesions strike chelonians in poor water conditions.
Watch for these species-specific illnesses:
- Respiratory problems in 20–40% of lizards with inadequate ventilation
- Fungal infections like aspergillosis in 6–12% of bearded dragons
- Metabolic disorders causing skeletal deformities in 18–24% of calcium-deficient young reptiles
- Mycoplasma infections in 10–15% of tortoises in multi-keeper settings
Your reptile’s species determines its disease risks.
Diagnostic Methods for Reptile Illness
When your reptile shows signs of illness, your veterinarian will rely on several key diagnostic tools to pinpoint the problem. Each method fulfills a distinct purpose—some reveal internal issues you can’t see, while others identify specific pathogens causing infection.
Understanding these approaches helps you know what to expect during your pet’s veterinary visit and why certain tests matter for accurate treatment.
Physical Examination and History
When you bring your scaled companion to a veterinarian, the consultation begins with thorough medical history and clinical signs documentation. History-taking accuracy boosts diagnostic techniques yield by roughly 20% when you report enclosure parameters—temperature, humidity, substrate—alongside symptoms.
Your observations of reptile behavior, appetite, bathroom habits, and mobility guide the health assessment, informing whether imaging or laboratory tests become necessary for proper veterinary care and reptile medicine intervention.
Bloodwork and Imaging (Radiographs)
Once clinical signs point toward systemic illness, bloodwork and imaging become your next diagnostic techniques. Reptile hematology and serum biochemistry reveal hidden metabolic disorders—calcium below 8 mg/dL flags metabolic bone disease, while uric acid over 10 mg/dL suggests renal failure. Radiographic imaging detects skeletal abnormalities, organomegaly, and foreign bodies in 45% of cases, strengthening veterinary care and disease prevention through early intervention.
- Hematology findings like anemia or elevated heterophils indicate infection or chronic illness
- Calcium-to-phosphorus ratios below 1:1 signal nutritional imbalances or kidney dysfunction
- Elevated AST levels exceeding 250 IU/L point to hepatic or muscular damage
- Radiographs uncover bone loss (30–80% in metabolic bone disease), egg binding, or fractures
PCR and Culture-Based Pathogen Identification
When radiographs don’t identify the culprit, molecular and microbiological tools step in. PCR sensitivity exceeds 90% for common viral and bacterial agents, delivering results in 24–72 hours—critical for infectious diseases where time matters.
Culture methods isolate viable pathogens, enabling antimicrobial susceptibility testing that guides targeted therapy.
Together, these diagnostic yield boosters improve pathogen detection while biosafety protocols protect your team during sample handling in reptile care and management.
Effective Treatment Options for Reptile Diseases
Once you’ve identified what’s wrong with your reptile, treatment becomes a careful balance of medical intervention and environmental adjustment. Your vet will tailor the approach based on your pet’s specific diagnosis, species, and overall condition.
The most effective treatments customarily draw from four core strategies that work together to restore health and prevent relapse.
Antimicrobial and Antiparasitic Therapy
When bacterial infections strike your reptile, targeted antimicrobial therapy becomes essential. Broad-spectrum antibiotics are often used initially—empiric treatment occurs in 62% of cases—but culture-guided regimens improve therapy outcomes markedly.
For parasite control, fenbendazole and praziquantel offer proven efficacy, though careful drug dosage matters since reptiles metabolize medications differently than mammals.
Antimicrobial resistance is rising in some pathogens, making proper infection management and species-specific treatment options increasingly critical.
Fluid and Nutritional Support
When infection management isn’t enough, your reptile needs more. Fluid therapy—oral or subcutaneous—restores hydration in 36% of ill reptiles, boosting survival by up to 40%.
Enteral feeding and parenteral nutrition deliver precise calories for disease prevention and treatment, supporting recovery through the reptile digestive system.
Combine these with calcium and vitamin supplementation to counteract nutritional disorders, stabilize weight within two weeks, and watch your companion regain strength.
Surgical Intervention
When medical management fails, surgical intervention becomes necessary—but it carries real stakes. Anesthesia risks in reptiles range from 0.5% to 3.0% mortality, while postoperative care demands precise temperature control and humidity.
Minimally invasive techniques boost recovery rates to 66%, with most reptiles returning to normal activity within 1–6 weeks. Your veterinary medicine team will guide you through foreign body removal, tumor excision, or fracture repair to restore reptile health.
Environmental and Husbandry Corrections
Before you reach for another prescription, look at the cage—that’s often where recovery begins. Temperature control, humidity management, and lighting systems aren’t optional; they’re medicine.
- Optimizing basking zones and UV-B exposure cuts metabolic bone disease incidence by 27% in captive tortoises
- Enclosure design improvements reduce respiratory infections by 30% when species-specific humidity targets are met
- Ventilation optimization and substrate changes lower dermatitis by 12–28%, supporting reptile nutrition and diet
- Creating a healthy environment through proper reptile husbandry reverses many chronic conditions without pharmaceuticals
Preventing Reptile Illness and Promoting Recovery
Prevention is always easier than cure, especially when you’re working with animals that hide their discomfort until it’s serious. Most reptile illnesses trace back to environmental missteps—wrong temps, poor lighting, inadequate nutrition—that compromise immune function before pathogens ever take hold.
Let’s walk through the core husbandry practices that keep your reptile healthy and support recovery when illness does strike.
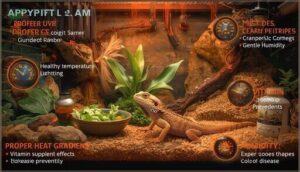
Optimal Housing, Heat, and Humidity
Your reptile’s housing isn’t just a box—it’s a life-support system. Temperature control with proper heating options creates 10–15°C gradients that support thermoregulation, while humidity management maintains species-appropriate levels (20–90% depending on origin).
Enclosure design paired with UVB lighting systems can reduce metabolic bone disease by 40%. Master these environmental factors, and you’ll prevent most husbandry-related illnesses before they start.
Proper Diet and Nutrition
Diet is the foundation of reptile health, yet many owners unknowingly create nutritional deficits that lead straight to illness. Proper reptile nutrition demands attention to species-specific needs, calcium intake, and food variety to prevent metabolic bone disease and immune compromise.
Your reptile care checklist for ideal husbandry:
- Nutrient Balance: Maintain calcium-to-phosphorus ratios of 1.5–2:1 for herbivores, closer to 1:1 for carnivores, with appropriate vitamin D3 supplementation when UVB exposure falls short.
- Dietary Supplements: Add calcium without excess phosphorus, adjusting for species and life stage—juveniles need daily feeding; adults thrive on 2–3 times weekly.
- Hydration Management: Provide consistent water access and monitor for dehydration signs like sunken eyes or skin tenting, which accelerate disease progression.
Master these diet fundamentals, and you’ll support sturdy reptile health from the inside out.
Hygiene and Quarantine Practices
Think of your enclosure as a sterile field—every new arrival poses a contamination risk until proven otherwise. Quarantine protocols reduce pathogen introductions by 34% when you isolate newcomers for 14–21 days in dedicated spaces with separate cleaning equipment.
During quarantine, conduct disease screening (fecal exams, baseline health checks) and maintain strict hygiene standards and environmental controls to prevent zoonotic diseases and protect your collection’s reptile health.
Monitoring and Early Intervention
You won’t always catch reptile illness in time unless you’re watching for early warning signs. Weekly health checks identify problems 1.6 times faster than monthly ones, while telemetry systems detect temperature and humidity shifts 60% earlier.
Proactive screening and veterinary intervention within 24–72 hours cut hospitalization by 22%, proving that vigilant reptile care transforms outcomes before common reptile health issues escalate.
Frequently Asked Questions (FAQs)
What are four signs of illness or disease in a reptile?
You’ll notice lethargy signs like reduced activity in 60% of cases, appetite changes affecting 70% of metabolic bone disease patients, weight loss in 55% with parasites, and droopy eyes alongside skin lesions signaling infection.
What are some of the signs of ill reptilian health?
You’ll notice lethargy, reduced appetite, abnormal bathroom habits, and altered mobility when your reptile isn’t well.
Behavioral shifts like hiding, drooping posture, or disengagement from their environment signal that veterinary attention is needed.
What are the symptoms of Amoebiasis in reptiles?
When amoebic colitis strikes, you’ll see chronic reptile diarrhea—often with mucus—alongside abdominal swelling and intestinal distress. Weight loss, lethargy, and anorexia commonly follow.
Fecal testing confirms parasitic infections, enabling targeted amebiasis treatment.
What are the symptoms of herpesvirus in reptiles?
Herpesvirus in reptiles manifests through vesicular lesions on the mouth or skin, mucous discharge, conjunctivitis, and occasionally respiratory distress.
You might observe oral plaques, facial swelling, or nasal discharge depending on your reptile’s species.
How can reptiles recover from stress-related illnesses?
When your reptile’s appetite drops by 62% under stress, recovery hinges on environmental optimization. This includes stabilizing temperature within ±2°C, ensuring proper humidity, providing fluid therapy, nutritional support, minimal handling, and behavioral enrichment.
Alongside these measures, targeted veterinary care is essential for reptile rehabilitation.
What are signs of reproductive system disorders?
Your female lizard or snake may show persistent vulvar swelling, abdominal distention, or egg binding—signs pointing to reproductive ultrasound findings like ovarian neoplasia, uterine prolapse, or hormonal imbalance requiring immediate veterinary attention.
How does dehydration affect reptile health?
Water loss isn’t always obvious—you’ll first notice sunken eyes, wrinkled skin, and tacky mucous membranes.
Dehydration signs disrupt fluid balance and thermal stress, compromising reptile health through electrolyte imbalance and weakened immunity.
What are common causes of reptile weight gain?
Obesity often stems from excess calories, limited activity, and suboptimal temperatures that slow metabolism.
Hormonal imbalances, metabolic disorders like hepatic lipidosis, and inadequate UVB exposure disrupting calcium metabolism can also contribute to weight gain.
How do temperature fluctuations impact reptile immunity?
When your pet’s enclosure swings more than 5°C daily, immune response weakens—stress hormones rise, white blood cells falter.
Temperature variance disrupts reptile resilience, making thermal stress a hidden threat to immune system health.
Can reptiles transmit diseases to humans?
Yes, reptiles carry zoonotic risks—particularly Salmonella—that can cause human infections. Up to 60% of cases affect children under five. Proper reptile hygiene and handwashing reduce disease transmission markedly.
Conclusion
The next time your reptile refuses food or retreats from interaction, you’ll know what others miss: illness doesn’t announce itself with drama—it whispers through posture, breathing patterns, and behavioral shifts invisible to untrained eyes.
Your ability to recognize reptile illness symptoms and treatment protocols determines whether minor deficiencies escalate into irreversible damage. Stay vigilant, trust your observations, and act decisively when those whispers demand your attention.
- https://www.merckvetmanual.com/all-other-pets/reptiles/disorders-and-diseases-of-reptiles
- https://www.anapsid.org/lethargy.html
- https://bvajournals.onlinelibrary.wiley.com/doi/10.1136/inp.h5633
- https://www.vin.com/apputil/content/defaultadv1.aspx?pId=25844&catId=150704
- https://www.vetfolio.com/learn/article/reptiles-performing-a-physical-examination