This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.

The venom, a toxic mix of proteins, works fast to damage tissues, disrupt your blood flow, and sometimes even interfere with breathing.
Symptoms can include nausea, dizziness, and severe pain.
Swift medical attention is essential, as antivenom can stop the toxins from causing permanent damage or worse.
Don’t try old myths like sucking out the venom—they just waste precious time.
Want to stay safe? Knowing their habits and habitats can strike fear out of the equation!
Table Of Contents
- Key Takeaways
- Rattlesnake Bite Overview
- What Happens When a Rattlesnake Bites
- Rattlesnake Bite Symptoms and Signs
- First Aid and Emergency Response
- Rattlesnake Bite Treatment and Management
- Rattlesnake Bite Prevention and Safety
- Rattlesnake Bite Statistics and Risk
- Rattlesnake Identification and Characteristics
- Rattlesnake Bite Recovery and Aftercare
- Rattlesnake Bite Emergencies and Complications
- Frequently Asked Questions (FAQs)
- What are the symptoms of a rattlesnake bite?
- What happens if you bite a rattlesnake?
- How long does it take a rattlesnake to bite you?
- How did a rattlesnake bite a man?
- Why is my rattlesnake biting me?
- Do rattlesnakes always rattle before biting?
- What happens when a rattlesnake bite?
- What are some interesting facts about rattlesnake bites?
- What part of the body do rattlesnakes bite most?
- Can someone survive a rattlesnake bite without treatment?
- Conclusion
Key Takeaways
- You’ll feel sharp pain, swelling, and see fang marks immediately after a rattlesnake bites, often followed by nausea, dizziness, or trouble breathing—get help fast.
- Don’t try outdated myths like sucking venom, using ice, or cutting the wound—these only make things worse. Immobilize the limb and call for medical assistance immediately.
- Antivenom is your best defense against the venom’s effects, as it neutralizes toxins and prevents severe complications like tissue damage, blood disorders, or organ failure.
- Rattlesnakes often give a warning rattle, but they can strike without it—spot their triangular heads, camouflaged patterns, and coiled postures to avoid close encounters.
Rattlesnake Bite Overview
When a rattlesnake bites, its venom enters your body through two sharp fang marks, causing immediate pain, swelling, and possible tissue damage.
Knowing the symptoms and acting fast can make all the difference in preventing serious complications.
Symptoms and Effects
Rattlesnake bites pack a punch, delivering venom that causes sharp, burning pain and swelling almost instantly.
Here’s what to know:
- Local Symptoms: Severe pain, redness, and potential tissue damage at the bite site.
- Systemic Effects: Nausea, dizziness, and difficulty breathing can quickly follow.
- Quick Escalation: Symptoms rattlesnake bite effects intensify fast—don’t wait, get medical help immediately!
Prepare for snake venom’s toxicity levels to hit hard.
Identification and Warning Signs
How do you know danger’s lurking?
That spine-tingling rattle sound is your first clue—nature’s no-nonsense warning.
Look for snake warning signs: a triangular head, tail vibrations, and patterns that blend into rocks or brush.
Understanding rattlesnake facts is essential for identifying these signs.
Still unsure? A table might help:
| Warning Signs | Examples |
|---|---|
| Sounds | Rattle noises, tail shaking |
| Body Language | Coiled posture, raised head |
| Venom Detection Clues | Snake bite symptoms timeline: redness, swelling, puncture marks |
Spot these cues and back off—quickly!
Importance of Medical Attention
Getting bitten by a rattlesnake isn’t the time for guesswork—it’s time for medical response.
Snake bites deliver venom that works fast, so you’ve got to move faster.
Don’t wait; rapid intervention with emergency care makes all the difference, especially for rattlesnake venom.
Antivenom is your lifeline, neutralizing toxins before they wreak havoc.
Every minute counts, so prioritize rattlesnake bite treatment immediately.
Ignoring symptoms or delaying treatment risks serious complications.
Simply put, medical assistance isn’t optional—it’s survival.
Call for help, now.
What Happens When a Rattlesnake Bites
When a rattlesnake bites, its venom quickly spreads from the puncture wounds, causing immediate pain, swelling, and tissue damage.
This venom, packed with toxic proteins, can disrupt your blood flow and nervous system, leading to serious systemic effects if untreated.
Immediate Pain and Swelling
When venom sinks in, that rattlesnake bite pain hits hard—like a blazing fire under your skin.
The swelling? It’s quick, fierce, and hard to miss.
You’ll spot fang marks at the center of it all, surrounded by puffiness that spreads fast.
Venom effects, like burning and tenderness, vary based on where you’re bitten.
Focus on wound care and swift emergency response!
Systemic Effects and Reactions
When a rattlesnake bites, it’s not just a local problem—it’s like flipping your body’s panic switch.
You could feel nausea, vomiting, or even struggle to breathe.
The venom messes with blood clotting, sparking blood disorders or organ failure if left untreated.
Nerve responses may falter, making muscles weak or numb.
Your immune reaction can spiral, causing swelling or shock.
The systemic effects of rattlesnake venom toxicity aren’t something you can shrug off—antivenom treatment is your lifesaver.
Venom Composition and Toxicity
Packed with toxic compounds, rattlesnake venom is a cocktail of proteins that wreak havoc on your body.
Its composition varies by species, delivering venom potency customized for killing prey or defense.
Rattlesnakes inhabit diverse environments across the Americas, as detailed on this rattlesnake facts webpage.
This venom can destroy tissue, mess with blood clotting, and even paralyze muscles.
Snake venom effects start fast, making quick medical attention vital to counter rattlesnake venom toxicity.
Rattlesnake Bite Symptoms and Signs
When a rattlesnake bites, you’ll usually feel intense pain and see swelling around the bite pretty quickly.
Other symptoms like dizziness, nausea, or trouble breathing can sneak up on you soon after, so it’s important to act fast.
Localized Effects and Wound Characteristics
Two fang marks and rapid rattlesnake bite swelling are your first clues.
The bite area may throb and bruise, resembling a painful watercolor.
Skin lesions or blisters can form, signaling venom absorption.
Watch for tissue damage—dead skin increases risk for wound infection or scarring.
Scars from deep injuries, even scar tissue after rattlesnake bite, remind you healing isn’t quick.
Systemic Effects and Organ Damage
When rattlesnake venom spreads, it’s like a system override with chaos released.
Organ damage and serious issues like organ failure can kick in fast.
The venom’s toxicity causes:
- Blood clots, or worse, a life-threatening lack of clotting.
- Nerve damage, messing with signals in key areas.
- Respiratory distress, making it harder to breathe.
- Tissue breakdown that weakens entire systems.
Immediate help is critical!
Common Symptoms and Reactions
Snake bites aren’t just a “hurt-and-heal” situation—they pack a punch.
You’ll feel some serious bite reactions, starting with intense pain and rapid swelling that spreads like wildfire.
Here’s what to watch for:
- Burning pain where the venom enters.
- Swelling creeping beyond the bite.
- Nausea that might derail your day.
- Feeling lightheaded or dizzy.
- Weak, achy muscles slowing you down.
- Strange metallic taste in your mouth.
These snake bite symptoms need quick action.
Rattlesnake venom causes poison symptoms that can escalate fast, so fast, calm emergency response makes all the difference.
First Aid and Emergency Response
If a rattlesnake bites you, staying calm and acting fast is critical to reduce the venom’s impact.
Knowing how to immobilize the bite and get proper medical help can make all the difference in your recovery.
Washing The Wound and Immobilizing The Area
Snake bites turn chaos into a race against time, but staying calm helps you think straight.
Start with gentle wound cleaning using soap and water—skip old-fashioned venom removal methods; they don’t work.
Then focus on immobilizing the area.
Keep the limb still, ideally using a splint, and make sure it’s positioned below heart level.
These snake bite first aid steps slow venom spread, giving you a fighting chance before rattlesnake bite treatment begins.
Understanding snake first aid is essential for effective management and treatment of venomous bites.
Getting Medical Help and Antivenom Treatment
After immobilizing the bite, getting medical help fast makes all the difference.
Head to a hospital immediately—antivenom is the top-line defense against venomous snake bites.
Understanding antivenom treatment options is essential for effective care.
Here’s how it works:
- Time Matters: Aim for treatment within 30 minutes.
- Antivenom Dosage: Administered via IV, it neutralizes venom.
- Cost: Be aware—it’s pricey but lifesaving.
What Not to Do and Common Misconceptions
Regarding rattlesnake bites, well-meaning advice can backfire.
Forget the old movie tricks—you can’t suck venom out like a superhero.
Cutting the wound? It just opens a door for infection.
Ice might seem helpful, but it actually worsens tissue damage.
And tourniquets? They cut off blood flow completely, which the venom-laden tissue actually needs.
| Myth | Reality | Risk |
|---|---|---|
| Tourniquet use | Stops blood flow | Tissue damage |
| Venom sucking | Useless and unsanitary | Infection |
| Wound cutting | Invites infection | Severe complications |
| Ice application | Boosts tissue destruction | Slower recovery |
Stick to proper rattlesnake bite first aid.
Rattlesnake Bite Treatment and Management
If a rattlesnake bites you, getting proper treatment quickly is essential to stop the venom’s effects and prevent complications.
Antivenom, pain management, and careful wound care are all part of the process to help you recover safely.
Antivenom Therapy and Administration
When a rattlesnake bites, antivenom therapy is the go-to for venom neutralization.
Administered via IV, it stops the spread of rattlesnake venom and improves treatment outcomes.
Quick action guarantees better results!
- Dosage matters, with 4–6 vials or more based on severity.
- Commonly stocked in hospitals.
- Side effects? Rare, but allergic reactions can occur.
- Always prioritize immediate medical response.
Effective treatment often involves rattlesnake antivenom to counteract the venom effects.
Pain Management and Medication
Once antivenom kicks in, managing pain becomes the next big step.
Snake bites can hurt—a lot—so doctors often rely on pain relief to keep things manageable.
You might get opioids for severe pain, but they come with risks like drowsiness or addiction, so they’re prescribed carefully.
Other options include NSAIDs, which help reduce pain and swelling, or acetaminophen, a solid choice for mild discomfort if used within safe limits.
Here’s a quick breakdown:
| Medication Options | Benefits | Watch Out For |
|---|---|---|
| Opioids | Strong pain relief | Addiction, drowsiness |
| NSAIDs | Reduce pain & swelling | Stomach irritation, bleeding |
| Acetaminophen | Mild pain relief | Liver damage (overuse) |
| Nerve Blocks | Precise relief | Limited availability, possible tingling |
| Ice Packs (adjunctive) | Soothes swelling | Temporary relief; not standalone |
Always follow your doctor’s recommendations for safe snake bite treatment.
Wound Care and Infection Prevention
Keeping the bite clean is step one in the rattlesnake bite wound healing process.
Here’s how:
- Wound Cleaning: Gently rinse with clean water; avoid vigorous scrubbing.
- Infection Control: Cover with a sterile bandage to block bacteria.
- Bacterial Prevention: Watch for redness or pus.
- Antibiotic Use: Let doctors decide.
- Skin Regeneration: Quick care speeds healing—no shortcuts!
Neglecting infection risks isn’t worth it.
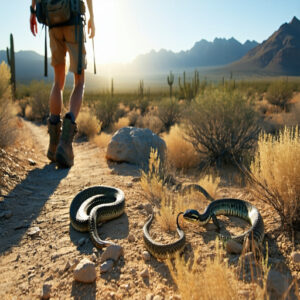
Rattlesnake Bite Prevention and Safety
You can avoid rattlesnake bites by wearing thick boots, sticking to trails, and staying alert in their habitats.
Understanding their behavior and giving them space keeps both you and the snake safe.
Wearing Protective Clothing and Gear
Don’t let your wardrobe leave you vulnerable—suit up smart for rattlesnake bite prevention.
Snake-proof boots and protective suits shield your lower legs, while venom guards provide extra bite resistance.
Toss on safety glasses to avoid surprises from low branches or tall grass.
When hiking, investing in Snake Proof Boots can substantially enhance overall safety.
- Stick to durable hiking gear designed for rugged outdoor use.
- Opt for thick, loose fabrics to block fang strikes.
- Prioritize ankle-coverage for rattlesnake bite safety.
Staying on Trails and Avoiding Disturbance
While protective clothing helps, your outdoor awareness matters just as much.
Here’s why trail safety tips make a difference:
| Action | Benefits | Risk Level |
|---|---|---|
| Stay on marked paths | Clear visibility, maintained ground | Low |
| Watch where you step | Spot snakes before close contact | Medium |
| Keep noise reasonable | Alert snakes to move away | Low |
You’ll find this simple hiking etiquette helps with snake avoidance – they’re typically more scared of you than you’re of them.
Understanding snake handling safety is essential for preventing bites and ensuring a safe outdoor experience.
Understanding Snake Behavior and Habitat
Your wild backyard’s venomous reptiles follow strategic habitat selection patterns.
From desert outcrops to forest edges, you’ll find different rattlesnake species adapting to their surroundings.
In warmer months, they’re solitary hunters, but winter brings them together in snake denning communities.
Understanding their geographic distribution – from the Southwest’s arid zones to the Southeast’s woodlands – helps you predict and avoid potential encounters with rattlesnake species.
Rattlesnake Bite Statistics and Risk
You’re more likely to win the lottery than die from a rattlesnake bite, with only five deaths among the 7,000 to 8,000 people bitten annually in the United States.
While getting bitten isn’t cheap – antivenom can cost up to $2,200 per vial, and severe cases might need over 100 vials – you’ll be relieved to know that with prompt medical treatment, your chances of survival are over 99%.
Frequency and Severity of Bites
After all that safety talk, here’s what the numbers tell us about bite frequency and severity factors.
| Time Period | Bite Patterns | Severity Level |
|---|---|---|
| Spring | Rising Cases | Moderate |
| Summer | Peak Activity | Highest Risk |
| Fall | Declining | Moderate |
| Winter | Lowest Cases | Minimal |
U.S. bite statistics show you’ve got about a 1 in 50,000 chance of encountering trouble – roughly 7,000-8,000 bites happen yearly.
While rattlesnake bite severity varies with venom levels, modern antivenom treatment means only 5-6 cases prove fatal.
High-Risk Groups and Demographics
Understanding who’s most at risk can help you stay safer.
The latest rattlesnake bite statistics reveal some clear patterns among vulnerable populations:
| Risk Group | Percentage | Main Cause |
|---|---|---|
| Rural Residents | 71% | Limited healthcare access |
| Male Population | 74-87% | Risk-taking behavior |
| Outdoor Workers | 53-70% | Daily exposure |
Age factors play a big role too – your kids need extra attention outdoors.
If you’re working farms or construction, you’re in the high-risk category.
While urban encroachment brings more encounters, rural residents face the biggest challenges with emergency care.
Mortality Rates and Survival Chances
Let’s examine the real odds of surviving a rattlesnake bite in America.
While these encounters can be scary, your survival chances are incredibly high – only 5-6 people out of 7,000-8,000 annual bites don’t make it.
The factors that impact survival are outlined in the following table:
| Factor | Impact on Survival |
|---|---|
| Quick Treatment | 99% survival rate |
| Delayed Help | Higher risk of death |
| Age | Kids/elderly most vulnerable |
| Location | Urban areas safer |
Most deaths happen because people wait too long to get help or have other health issues. The secret to beating these odds? Don’t hesitate to call 911 – modern antivenom is incredibly effective when you get it fast, and this can significantly improve your survival chances.
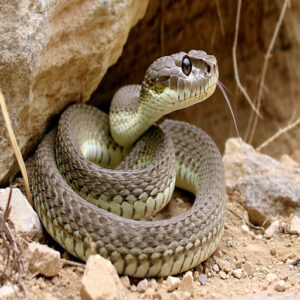
Rattlesnake Identification and Characteristics
You’ll spot a rattlesnake by its triangular head, diamond-shaped markings down its back, and that famous warning rattle at its tail tip.
While they’re found throughout the United States, you’re most likely to encounter these pit vipers in dry, rocky areas where they can reach lengths up to 8 feet, though most are much shorter.
Snake Recognition and Warning Signs
Spotting a rattlesnake feels like nature’s alarm clock jolting you awake.
To avoid trouble, watch for these signs:
- Snake Identification: Broad, triangular heads with slit-like pupils.
- Venom Detection: Heat-sensing pits near their nostrils.
- Rattle Sounds: A sharp, buzzing noise.
- Snake Behavior: Coiled and motionless near rocks or brush.
- Warning Signals: Defensive rattling when threatened.
Stay calm—rattlesnakes prefer slithering away over confrontation.
Fang Marks and Venom Effects
You’ll spot fang marks as two punctures—nature’s syringe from a venomous snake.
Rattlesnake fangs fold when idle but snap forward to inject snake venom, causing damage ranging from swelling to necrosis.
| Feature | Details |
|---|---|
| Venom Delivery | Fangs inject toxin fast |
| Fang Structure | Retractable, sharp |
| Rattle Sounds | Defensive warning |
| Venom Potency | Varies by snake species |
Stay sharp—it’s no game with rattlesnake fangs!
Habitat and Geographic Distribution
You’ll find rattlesnakes thriving in desert ecosystems, rocky terrain, and mountain areas, where they bask in warmth and hunt.
Their geographic range spans North and South America, from Arizona’s sunny deserts to the dense Texas brush.
They’re adaptable creatures, equally at home in wild habitats like forests, grasslands, and even near swamps.
Knowing their rattlesnake habitat—like warm rocky areas and deserts—helps you avoid unwanted encounters.
Always watch your step where nature likes to hide surprises!
Rattlesnake Bite Recovery and Aftercare
Recovering from a rattlesnake bite takes time, medical care, and careful monitoring to avoid complications.
You’ll need to follow your doctor’s instructions closely, since proper aftercare can make all the difference in preventing long-term issues like nerve or tissue damage.
Healing Process and Timeline
Healing from a rattlesnake bite isn’t a sprint—it’s a careful process.
Recovery time depends on treatment, focusing on pain management, wound healing, and tissue regeneration.
Proper care minimizes scarring, and it is crucial to keep an eye on rattlesnake bite symptoms as the wound evolves.
Medical guidance is key, especially with venom removal and infection prevention.
Comparing rattlesnake bite pictures of stages can help you gauge progress, but patience (and a good story) pays off.
Effective snake wound care is vital for a successful recovery from a venomous snake bite.
Potential Long-Term Effects and Complications
Sometimes, a rattlesnake bite leaves behind more than scars—think nerve damage, chronic pain, or even organ failure.
These long-term effects can sneak in, making recovery from rattlesnake bite treatment feel like a marathon, not a sprint.
Here’s what might linger:
- Tissue loss or scarring, leaving permanent reminders.
- Health complications, like weakened muscles or recurring numbness.
- Persistent side effects of rattlesnake bite, including skin peeling or discoloration.
- Rare cases of organ damage requiring ongoing care.
It’s essential to have a rattlesnake bite kit for emergency situations to minimize potential harm.
Stay vigilant and prioritize follow-up care!
Follow-Up Care and Medical Monitoring
Recovering from a rattlesnake bite takes time and effort.
Here’s how to stay on top of it:
- Wound Healing: Watch for redness, swelling, or unusual pain—these can signal infection.
- Medical Checkups: Keep doctor appointments to track progress and adjust recovery plans.
- Post Bite Care: Discuss lingering symptoms or possible long-term effects like tissue damage during follow-ups.
Stay proactive for smooth recovery!
Rattlesnake Bite Emergencies and Complications
When a rattlesnake bite turns serious, you’ll need to act fast to handle life-threatening issues.
Recognizing emergency signs and getting immediate medical help can make all the difference in preventing complications.
Signs of Anaphylaxis and Shock
When venom spreads, it can trigger allergic reactions or shock symptoms fast.
Look for signs like hives, swelling, throat tightness, or feeling woozy.
Breathing hard? That’s no joke—anaphylaxis treatment, like epinephrine, is essential.
Keep your eyes open for confusion or dizziness too.
A rattlesnake bite’s venom response can spiral into an emergency.
Swift snake bite first aid means stopping these symptoms before things get worse.
Trust your gut, and act quickly.
When to Call 911 and Seek Immediate Help
Panic won’t help, but calling 911 might save a life.
If you notice rattlesnake bite symptoms like extreme swelling, breathing trouble, or even fainting, it’s time for an emergency response.
Share where the bite happened and how long ago—it’s key info for urgent care.
Antivenom can counter dangerous venom effects, but getting to a trained professional fast is critical.
Waiting increases the bite severity and risks serious complications.
Keep calm, avoid walking too much, and let the responders handle the hard stuff.
Quick action could make all the difference.
Managing Severe Reactions and Allergic Responses
When a severe reaction kicks in, like struggling to breathe or feeling a rapid, weak pulse, it’s time to act fast.
Here are critical signs:
- Difficulty breathing or muscle weakness from venom toxicity.
- Severe swelling and symptoms of allergic shock.
- Neurotoxic effects needing immediate antivenom.
For anaphylaxis treatment, epinephrine is life-saving.
Quick emergency response prevents venom from causing lasting damage.
Don’t gamble—treat snake bite symptoms seriously when every second counts.
Frequently Asked Questions (FAQs)
What are the symptoms of a rattlesnake bite?
You’ll feel sharp pain and swelling at the bite, often with nausea, dizziness, or trouble breathing.
The area may redden and swell fast.
Sometimes, there’s a metallic taste, tingling, or lightheadedness.
Seek help immediately!
What happens if you bite a rattlesnake?
If you bite a rattlesnake (which, let’s be honest, is a terrible idea), nothing harmful happens to you unless venom gets in your mouth.
Their venom is designed to inject, not absorb through their skin.
How long does it take a rattlesnake to bite you?
In the blink of an eye, a rattlesnake can strike and bite, usually under half a second.
It’s a lightning-fast reflex, blending speed and precision, leaving little time to react if you’re too close.
How did a rattlesnake bite a man?
You might be hiking or stepping near rocky spots when one lashes out lightning-fast, usually in defense.
It detects your movement or vibration, strikes with folded fangs unfurling, injecting venom in milliseconds.
Why is my rattlesnake biting me?
It’s likely your rattlesnake feels stressed, threatened, or startled.
Maybe it’s sensing unfamiliar handling or abrupt movements.
Stay calm, adjust your approach, and give it space to relax—respect wins over defensive fangs every time.
Do rattlesnakes always rattle before biting?
They don’t always rattle first.
Sometimes they strike without warning, especially if startled or feeling cornered.
The rattle’s like an alarm system, but snakes skip it when they think a quick escape or defense is better.
What happens when a rattlesnake bite?
When one sinks its fangs into you, venom immediately targets your blood and tissues, causing pain, swelling, and serious symptoms like nausea or breathing trouble.
Stay calm, act fast, and get medical help—it’s a real emergency!
What are some interesting facts about rattlesnake bites?
You’d be surprised—only about 20-25% of rattlesnake bites are “dry” with no venom.
Symptoms hit fast—pain, swelling, or even breathing trouble.
Funny enough, baby rattlesnakes aren’t deadlier; adults control venom better.
What part of the body do rattlesnakes bite most?
You’d think rattlesnakes aim for exposed skin, right?
Actually, they most often bite hands, arms, feet, or ankles—basically anywhere you’re reaching or stepping.
So, watch where you put your hands and feet!
Can someone survive a rattlesnake bite without treatment?
You’ve got a slim chance of surviving without treatment, but it’s risky.
The venom can cause severe tissue damage, organ failure, or death.
Seeking quick medical attention, especially antivenom, is your best shot at survival.
Conclusion
A rattlesnake bite is like nature’s harsh wake-up call, demanding swift action.
You’ll face intense pain, swelling, and possibly life-threatening symptoms as the venom works quickly.
Knowing what happens when a rattlesnake bites, along with the symptoms and facts, can save valuable time.
Always seek medical attention immediately—antivenom is key to recovery.
Stay prepared by understanding snake behavior, habitats, and prevention methods.
A little knowledge can make all the difference when it matters most.