This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.
A single bite from an Acanthophis death adder delivers a biochemical assault so precise that it can shut down your body’s communication network within hours—yet you might not feel the strike until paralysis has already begun.
Death adder neuromuscular blocking toxins represent one of nature’s most complex weapons: a cocktail of presynaptic phospholipase A2 complexes and postsynaptic alpha-neurotoxins that attack the neuromuscular junction from multiple angles simultaneously.
Unlike many venoms that cause immediate pain or tissue destruction, these molecules work silently, dismantling the mechanisms that allow your muscles to contract—starting with drooping eyelids and slurred speech, then progressing to respiratory failure if left untreated.
Understanding how these toxins differ across species, why some victims experience rapid paralysis while others deteriorate slowly, and why antivenom works brilliantly in certain cases but fails in others requires examining the molecular choreography at nerve terminals.
Table Of Contents
- Key Takeaways
- What Are Death Adder Neuromuscular Toxins?
- Mechanisms of Neuromuscular Blockade
- Effects on The Neuromuscular Junction
- Clinical Manifestations of Neurotoxicity
- Treatment Strategies for Neuromuscular Toxicity
- Frequently Asked Questions (FAQs)
- Is there anti-venom for death adder?
- How toxic is a death adder?
- What toxins affect the nervous system?
- Which snake venom is responsible for neurotoxicity?
- How does death adder venom work?
- Are adders neurotoxic?
- What does snake venom do to the neuromuscular junction?
- Does snake venom contain paralyzing toxins?
- How dangerous is a death adder snake bite?
- What are the chances of survival?
- Conclusion
Key Takeaways
- Death adder venom deploys a dual-mechanism attack at the neuromuscular junction through presynaptic phospholipase A2 toxins that irreversibly destroy nerve terminals and postsynaptic alpha-neurotoxins that competitively block acetylcholine receptors, creating paralysis patterns that differ dramatically in onset speed and reversibility.
- Antivenom cannot reverse established neuromuscular blockade from presynaptic toxins because these molecules cause permanent structural damage to nerve terminals requiring weeks of regeneration, while postsynaptic toxin effects may respond to antibody neutralization if administered before complete receptor occupation occurs.
- Clinical presentation progresses predictably from subtle cranial nerve dysfunction (ptosis, diplopia, dysphagia) within hours to descending flaccid paralysis affecting proximal limbs, bulbar muscles, and ultimately respiratory muscles, with mechanical ventilation becoming the critical life-sustaining intervention when antivenom fails to halt progression.
- Significant venom compositional variation exists across Acanthophis species and even among individual snakes within populations (up to 40% difference in single toxin family abundance), directly impacting clinical severity, paralysis timelines, and antivenom efficacy in ways that complicate standardized treatment protocols.
What Are Death Adder Neuromuscular Toxins?
Death adder venom isn’t a single weapon—it’s a complex cocktail of neurotoxins engineered to paralyze prey by attacking the neuromuscular junction where nerves meet muscles. When you understand what’s actually in this venom, you’ll see why bites cause such distinct patterns of paralysis and why treatment remains challenging even with antivenom available.
Like their cobra relatives, death adders rely on acetylcholine receptor blockade to immobilize victims, though their venom acts faster due to higher neurotoxin concentrations.
Let’s break down the key components you need to know about, starting with an overview of the venom itself, then moving through the major toxin families and how they vary across different death adder species.
Overview of Death Adder Venom
Death adder venom represents a complex biochemical weapon characterized by neurotoxicity as its primary envenoming syndrome. The venom composition includes presynaptic phospholipase A2 toxins, postsynaptic alpha-neurotoxins, and myotoxic enzymes, with significant toxin variability observed across Acanthophis species and geographic distribution.
This variability in venom potency and toxin proportions influences clinical presentation, antivenom efficacy, and the severity of neuromuscular blockade following envenoming. Additional background on the species’ venom, danger to humans, and recommended first aid can be found in this comprehensive Death Adder overview.
Major Toxin Classes in Death Adder Venom
You’ll encounter three primary toxin classifications in death adder venom composition: presynaptic phospholipase A2 complexes that irreversibly damage nerve terminals, postsynaptic alpha-neurotoxins that competitively block acetylcholine receptors, and myotoxins that degrade muscle fibers.
These components exhibit synergistic neurotoxin effects during envenoming, amplifying neuromuscular blockade beyond individual toxin activity and complicating antivenom management strategies in toxinology and envenoming management protocols.
For further details about the clinical effects and symptoms of death adder bites, additional reading is highly recommended.
Species Variations in Toxin Composition
You’ll find that venom variation across Acanthophis spp. reflects molecular adaptation shaped by toxin evolution and geographic patterns.
Species diversity drives distinct dominant toxin profiles—some death adder populations favor presynaptic phospholipase A2 complexes, while others express higher postsynaptic alpha-neurotoxin ratios.
Individual snakes within a species can differ by up to 40% in single toxin family abundance, complicating antivenom development and neurotoxicity prediction in clinical envenoming scenarios.
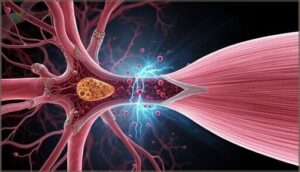
Mechanisms of Neuromuscular Blockade
Death adder venom doesn’t work through a single pathway—it attacks your neuromuscular junction from two distinct angles, each with its own molecular fingerprint and clinical timeline. Understanding these mechanisms isn’t just academic; it explains why some victims experience rapid paralysis while others deteriorate slowly, and why antivenom works brilliantly in some cases but fails in others.
Death adder venom attacks your neuromuscular junction from two distinct angles, explaining why paralysis patterns and antivenom responses vary dramatically between victims
You’ll see how presynaptic phospholipase A2 toxins dismantle nerve terminals from within, how postsynaptic alpha-neurotoxins block receptor sites like molecular padlocks, and why these differences matter when seconds count.
Understanding these mechanisms can help you recognize early symptoms and assess risk—especially if you’re exploring coral snake species profiles and bite protocols for regional safety.
Presynaptic Phospholipase A2 Toxins
You’re facing one of nature’s most insidious venom components when presynaptic phospholipase A2 toxins enter your neuromuscular junction. These neurotoxic peptides demonstrate devastating PLA2 activity through enzyme catalysis that triggers phospholipid hydrolysis, causing irreversible membrane disruption at motor nerve terminals.
The consequences unfold through four relentless stages:
- Toxin binding to presynaptic membranes rich in phosphatidylcholine
- Enzymatic degradation of critical membrane phospholipids
- Impaired vesicle cycling that cripples neurotransmitter release
- Persistent synaptic failure requiring nerve terminal regeneration
This presynaptic neurotoxicity explains why antivenom can’t quickly reverse established paralysis.
Postsynaptic Alpha-Neurotoxins
Unlike their presynaptic counterparts, postsynaptic alpha-neurotoxins in death adder venom composition achieve neurotoxicity through competitive receptor interactions at nicotinic acetylcholine receptors.
You’ll observe these neurotoxic peptides—containing 60 to 66 amino acids stabilized by disulfide bonds—block acetylcholine signaling through toxin binding at the neuromuscular junction, producing rapid flaccid paralysis during envenoming that antivenom can potentially reverse through improved antivenom efficacy and receptor displacement mechanisms.
Differences in Toxin Actions
The kinetics and reversibility of paralysis mechanism fundamentally distinguish presynaptic-acting neurotoxic peptides from their postsynaptic counterparts through distinct receptor dynamics and neurotoxin effects.
- Onset timing: Presynaptic neurotoxins produce gradual, delayed paralysis through vesicle depletion, while postsynaptic toxin binding creates rapid weakness within hours.
- Recovery duration: Presynaptic venom components require nerve terminal regeneration over days; postsynaptic effects may reverse as toxin interactions dissociate.
- Neurotoxicity pattern: Presynaptic blockade shows cumulative decline; postsynaptic causes immediate complete paralysis.
- Antivenom response: Circulating toxin neutralization helps postsynaptic cases more than established presynaptic neuromuscular damage.
- Clinical severity: Mixed profiles create biphasic paralysis requiring extended respiratory support and intensive monitoring.
Effects on The Neuromuscular Junction
When death adder venom reaches the neuromuscular junction, it doesn’t simply interfere with nerve signaling—it fundamentally disrupts the mechanisms that allow your muscles to contract and function.
The toxins work through distinct pathways, some preventing neurotransmitter release while others block the receptors themselves, creating a cascade of paralytic effects that vary in their reversibility. Understanding these specific effects at the molecular level clarifies why some patients recover quickly while others face prolonged respiratory support despite antivenom administration.
Disruption of Acetylcholine Release
When presynaptic neurotoxins from death adder venom reach your neuromuscular junction, they trigger synaptic failure by severely disrupting acetylcholine release. Toxin binding to nerve terminals impairs calcium regulation, reducing the calcium influx needed for vesicle dynamics and neurotransmitter release.
This creates profound neurotransmitter imbalance, depleting acetylcholine availability within minutes and initiating the progressive neurotoxicity that leads to paralysis.
Blockade of Nicotinic Receptors
Beyond the presynaptic disruption you’ve just learned about, death adder neurotoxins also include postsynaptic alpha-neurotoxins that target nicotinic receptors directly. Receptor binding by these neurotoxic agents creates channel blockade through competitive antagonism at acetylcholine sites, halting synaptic transmission and producing paralysis.
This neurotoxin action involves allosteric modulation and variable reversibility, with postsynaptic effects appearing within hours as presynaptic neurotoxins continue their irreversible nerve terminal damage.
Irreversible Vs. Reversible Paralysis
You’ll face two fundamentally different paralysis outcomes after death adder envenoming. Presynaptic phospholipase A2 neurotoxins produce irreversible nerve terminal destruction, causing neurotoxicity that persists despite antivenom administration, while postsynaptic alpha-neurotoxins create reversible competitive receptor blockade with variable paralysis recovery timelines.
- Irreversible paralysis demands weeks of respiratory support as nerve regeneration slowly restores function amid progressive muscle atrophy
- Neurotoxic effects from presynaptic toxins prevent antivenom from halting established paralysis at toxicity levels already damaging terminals
- Reversible neurotoxin effects offer hope through supportive care during the critical window before permanent envenoming consequences emerge
Clinical Manifestations of Neurotoxicity
When death adder venom enters your body, you’ll experience a predictable cascade of neuromuscular symptoms that demands immediate clinical recognition.
The presentation unfolds in distinct phases, beginning with subtle cranial nerve dysfunction and potentially advancing to life-threatening respiratory compromise. Understanding this temporal sequence is essential for timely intervention and ideal patient outcomes.
Early Neuromuscular Symptoms
You’ll notice the earliest neurotoxin effects within minutes to hours after envenoming, often beginning with subtle ptosis (eyelid drooping), blurred or double vision, and difficulty swallowing—hallmark signs of neuromuscular fatigue at cranial nerve terminals.
These initial manifestations of neurotoxicity signal acetylcholine transmission failure, progressing to bulbar weakness, limb muscle weakness, and intercostal muscle compromise, which precipitates respiratory failure if neurotoxic paralysis advances unchecked.
Progression to Flaccid Paralysis
As neurotoxin effects intensify, you’ll see muscle weakness advance through a predictable pathway, culminating in symmetrical descending flaccid paralysis that defines death adder envenoming.
The progression of neurotoxin effects can be outlined as follows:
- Proximal limb weakness emerges within 6 to 12 hours, affecting hip and shoulder girdle before hands and feet
- Neck and bulbar muscle involvement produces dysphagia and slurred speech as neurotoxicity deepens
- Intercostal muscle compromise reduces chest expansion and tidal volumes, signaling impending respiratory failure
- Plateau phase precedes autonomic symptoms, where paralysis stabilizes before potential recovery or progression
Respiratory Complications and Severity
Respiratory failure marks the most critical juncture in death adder envenoming. You’ll find airway failure develops as diaphragmatic and intercostal paralysis intensifies, progressing rapidly to respiratory arrest without ventilator support and oxygen therapy.
Neurotoxicity-induced hypoventilation triggers hypoxemia and hypercapnia, occasionally complicated by pulmonary edema. Antivenom halts progression but won’t immediately reverse established neuromuscular blockade, making timely respiratory intervention essential for survival.
Treatment Strategies for Neuromuscular Toxicity
When you’re facing death adder envenomation, treatment becomes a balancing act between what antivenom can realistically do and what your body needs to survive the paralysis.
The reality is that antivenom won’t magically reverse established neurotoxicity, so supportive care—especially respiratory management—becomes your lifeline. Let’s examine the current treatment approaches and where research is heading to address the gaps in managing these complex neuromuscular toxins.
Antivenom Mechanism and Limitations
Understanding antivenom efficacy requires you to recognize both its power and its limits in snakebite treatment. Though intravenous antibody infusion can neutralize circulating venom through antibody affinity binding, antivenom doesn’t reverse established neurotoxicity from death adder envenoming.
Critical limitations include:
- Presynaptic toxins cause irreversible nerve terminal damage
- Antibodies can’t effectively bind toxins already attached at neuromuscular junctions
- Venom variation across species affects toxin neutralization
- Hypersensitivity reactions complicate treatment outcomes
- Single-vial dosing may prove insufficient for severe envenoming
Supportive Care and Respiratory Management
When antivenom can’t undo established paralysis, you’ll need mechanical ventilation and respiratory support to survive. Rapid sequence intubation secures your airway as flaccid paralysis progresses toward respiratory failure, while lung-protective ventilator settings minimize barotrauma during prolonged ventilation.
Secretion clearance through chest physiotherapy and suctioning prevents mucus plugging, and early patient mobilization counters deconditioning—thorough supportive care that sustains life during neurotoxicity resolution.
| Intervention | Clinical Purpose | Specific Technique |
|---|---|---|
| Airway Management | Secure compromised airway | Endotracheal intubation with rapid sequence technique |
| Ventilation | Maintain oxygenation during paralysis | Lung-protective settings, capnography monitoring |
| Secretion Clearance | Prevent mucus plugging | Suctioning, chest physiotherapy, mucolytics |
| Monitoring | Track neuromuscular function | Pulse oximetry, arterial blood gas analysis |
| Patient Mobilization | Counter deconditioning | Progressive physiotherapy, DVT prophylaxis |
Future Directions in Therapeutic Research
Innovation in snakebite therapeutics targets presynaptic neurotoxicity through precision medicine and regenerative approaches. Gene therapy may repair nerve terminals damaged by venom’s neurotoxic peptides, while immune modulation could prevent irreversible paralysis.
Digital therapeutics enable real-time monitoring of neurotoxicity progression, optimizing antivenom timing and dosing. These therapeutic strategies for snakebite promise to overcome current antivenom limitations, potentially reversing established neuromuscular blockade.
Frequently Asked Questions (FAQs)
Is there anti-venom for death adder?
Yes, you’ll find CSL Death Adder Antivenom available—each vial contains 6000 units standardized to neutralize venom. It binds circulating toxins effectively, though established neurotoxicity won’t reverse immediately after administration.
How toxic is a death adder?
Death Adder venom potency ranks high among Australian snakes due to neurotoxicity that can cause flaccid paralysis and respiratory failure, though mortality rates remain low with prompt antivenom and supportive care managing severe envenoming effectively.
What toxins affect the nervous system?
Your nervous system faces attack from neurotoxic peptides that disrupt neurotransmitter block at the neuromuscular junction, causing nerve damage through toxin binding.
Presynaptic neurotoxins trigger envenoming by altering venom composition, producing severe neurotoxicity and neurotoxin effects.
Which snake venom is responsible for neurotoxicity?
Neurotoxicity from snake bites stems primarily from elapid family venoms, including death adders, cobras, kraits, and mambas. Their neurotoxic components block acetylcholine receptors and disrupt neurotransmitter release, causing progressive paralysis.
How does death adder venom work?
When you’re bitten, the venom floods your bloodstream with neurotoxins—presynaptic toxins block nerve signals from releasing acetylcholine, while postsynaptic toxins prevent muscles from receiving those signals, causing rapid paralysis.
Are adders neurotoxic?
Most victims—over 70% in documented cases—develop flaccid paralysis from death adder envenoming.
Your nervous system faces a targeted attack: neurotoxic venom disrupts acetylcholine signaling, causing progressive weakness and potential respiratory failure without antivenom.
What does snake venom do to the neuromuscular junction?
Death adder venom attacks your neuromuscular junction through dual toxins: presynaptic phospholipases that halt acetylcholine release from nerve terminals, and postsynaptic alpha-neurotoxins that block receptor sites, together causing progressive muscle paralysis.
Does snake venom contain paralyzing toxins?
Yes—snake venom composition includes paralytic neurotoxins that disrupt neuromuscular transmission, causing progressive paralysis symptoms.
Neurotoxic components target acetylcholine pathways at synapses, blocking signal reception and transmitter release, producing flaccid weakness requiring urgent treatment options.
How dangerous is a death adder snake bite?
Envenoming from this species represents a medical emergency requiring immediate intervention, as neurotoxic effects can progress rapidly to respiratory failure without prompt antivenom administration and supportive care including mechanical ventilation.
What are the chances of survival?
Your recovery odds improve dramatically with swift medical response and antivenom availability.
Venom dosage, bite location, and patient factors like age and health critically determine survival rates, though neurotoxicity requires intensive snakebite treatment.
Conclusion
Knowledge is the antidote to fear”—and understanding death adder neuromuscular blocking toxins transforms paralysis from mysterious threat into manageable medical emergency.
You’ve seen how presynaptic phospholipases and postsynaptic neurotoxins orchestrate silent shutdown of your neuromuscular junctions, why respiratory failure demands immediate intervention, and how antivenom specificity determines survival outcomes.
Armed with this molecular roadmap, you can recognize early symptoms, advocate for prompt treatment, and appreciate why supportive care bridges the gap between envenomation and recovery.
- http://www.graphpad.com/
- http://scholar.google.com/scholar?q=Snakes+across+the+Strait%3A+trans-Torresian+phylogeographic+relationships+in+three+genera+of+Australasian+snakes+%28Serpentes%3A+Elapidae%3A+Acanthophis%2C+Oxyuranus%2C+and+Pseudechis%29+Wuster+2005
- https://www.mja.com.au/journal/2004/181/11/snakebite-tropical-australia-prospective-study-top-end-northern-territory
- http://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0001841
- https://qjmed.oxfordjournals.org/content/qjmed/89/1/25.full.pdf