This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.

Your snake might struggle with unusual molting patterns or develop cloudy eyes, making it harder for them to see.
In more severe cases, the infection can invade deep tissues, causing painful ulcers, facial disfigurement, or swelling.
Left untreated, it spreads to essential organs like the lungs, potentially leading to pneumonia.
Watch for behavioral changes too, like lethargy or refusal to eat.
Early recognition is key to protecting your snake’s health—don’t wait for the infection to worsen before taking action.
Understanding the progression could save your pet’s life, and it’s crucial to be aware of these symptoms to ensure early recognition and take necessary actions to prevent the infection from spreading to essential organs.
Table Of Contents
- Key Takeaways
- Snake Fungal Disease Signs
- Early Infection Symptoms
- Severe Infection Symptoms
- Fungal Infection Diagnosis
- Advanced Disease Symptoms
- Frequently Asked Questions (FAQs)
- What are the symptoms of snake fungal disease?
- How do you treat a snake fungal infection?
- What are the symptoms of a serious fungal infection?
- What are the early stages of a fungal infection?
- How does snake fungal disease affect reproduction?
- What habitat conditions increase the risk of infection?
- Can snake fungal disease impact other reptiles?
- Are certain snake species immune to SFD?
- How does the disease affect snake behavior?
- Conclusion
Key Takeaways
- Watch for early signs like scabs, lesions, thickened skin, or abnormal molting patterns to catch the infection before it gets worse.
- Cloudy eyes, behavioral changes like lethargy, and facial swelling often point to a burgeoning fungal issue.
- Severe symptoms include ulcers, subcutaneous nodules, and internal damage to organs like lungs and liver, increasing risk of pneumonia.
- Clean, well-ventilated habitats and prompt veterinary attention can prevent and manage the disease effectively.
Snake Fungal Disease Signs
You’ll notice snake fungal disease through striking signs like scabs, lesions, and facial swelling.
Striking signs of snake fungal disease include scabs, lesions, and facial swelling, warning of a serious underlying infection.
As the infection worsens, symptoms can include cloudy eyes, subcutaneous nodules, and even disfiguring damage to the skin and tissues.
Localized Scabs and Lesions
When spotting snake fungal symptoms, localized scabs and lesions are telltale signs.
These crusty, thickened areas mark the infection site and highlight skin damage.
Watch out for:
- Crust appearance that disrupts smooth scales
- Localized thickening near affected areas
- Lesion severity varying from mild to severe
- Skin lesions that hinder natural molting
- Scabs indicating a slow healing process
Facial Swelling and Disfigurement
Facial swelling is one of the most noticeable snake fungal symptoms, often signaling severe infection stages.
Facial swelling signals severe stages of snake fungal disease, revealing disfiguring lesions that impede hunting, breathing, and overall survival.
The swelling’s diagnostic value lies in its link to disfiguring facial lesions, which can impact the snake’s ability to hunt or breathe.
As the infection worsens, disfigurement’s long-term effects become evident, raising ethical concerns about interventions and highlighting the critical severity of these facial disfigurements.
Cloudy or Opaque Eyes
Cloudy or opaque eyes are another hallmark snake fungal disease symptom. This eye opacity often points to infection severity and potential vision impairment.
You might notice:
- White, cloudy patches covering the eyes.
- Difficulty maneuvering or striking due to vision changes.
- Signs of eye infections worsening over time.
- Increased blindness risk without timely treatment options.
Ophidiomyces ophiodiicola is the cause of this condition. Prompt care helps minimize lasting damage, ensuring a better outcome with timely treatment.
Subcutaneous Nodules and Ulcers
While cloudy eyes hint at trouble, subcutaneous nodules and ulcers signal deeper tissue involvement.
These lumps, often firm and irregular, highlight nodule formation beneath skin lesions.
Ulcer development follows, exposing snakes to secondary infections and worsening tissue damage.
Proper identification of these symptoms can guide treatment options, helping manage snake fungal infection before it progresses to life-threatening stages.
Early Infection Symptoms
When a snake first shows signs of a fungal infection, you’ll notice subtle changes like unusual molting or small patches of thickened skin.
Early symptoms can also include cloudy eyes or minor skin ulcers, which may seem harmless but signal the need for prompt attention.
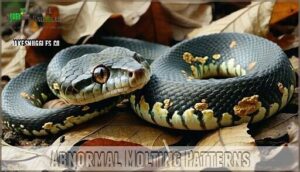
Abnormal Molting Patterns
When snakes face a fungal infection, abnormal molting patterns often appear, signaling trouble during shedding.
Watch for:
- Molting frequency changes beyond the norm.
- Incomplete sheds, leaving small patches stuck.
- Dysecdysis causes, such as stress or infection.
- Persistent shedding difficulties with retained layers.
- Skin retention worsened by underlying skin lesions.
These molting issues suggest early symptoms of snake fungal disease symptoms requiring prompt care.
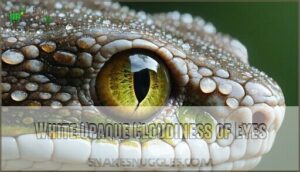
White Opaque Cloudiness of Eyes
Spotting white opaque cloudiness in the eyes could mean vision impairment, often signaling early snake fungal disease symptoms.
This specific trait shows how infection severity begins affecting eye structure and may lead to secondary infections.
| Symptom | Cause |
|---|---|
| Cloudy eyes | Early fungal infection |
| Vision issues | Tissue inflammation |
| Swollen appearance | Ophidian fungal damage |
| Secondary infections | Reduced immune defenses |
| Eye discoloration | Progression of symptoms |
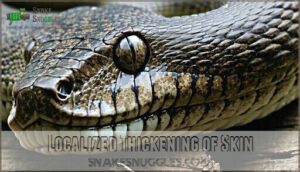
Localized Thickening of Skin
In the early stages of snake fungal disease, you might notice localized thickening of the snake’s scales.
This hardened, crusty skin often signals a developing snake skin infection. Lesion severity varies, but affected species can show pronounced rough patches over time.
Diagnostic imaging may help pinpoint these snake fungal signs, aiding timely intervention against worsening snake skin lesions.
Such infections can stem from inadequate sanitation practices within their enclosure.
Skin Ulcers and Nodules
Moving from thickened skin to deeper damage, snake skin infections often reveal ulcerations and nodule formation.
These snake fungal lesions can cause blisters and tissue damage, eventually leading to painful snake skin ulcers.
The healing process may slow as dermal infections progress, compromising the scales, and monitoring ulcer severity and addressing early signs like small nodules can dramatically improve outcomes for snakes showing these symptoms.
Severe Infection Symptoms
When a snake’s fungal infection worsens, the symptoms become increasingly severe and harder to manage.
You might notice deep tissue invasion, organ damage, or disfiguring facial lesions, all of which can substantially impact the snake’s health.
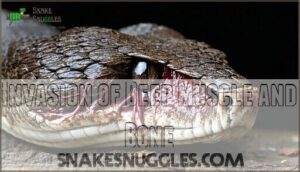
Invasion of Deep Muscle and Bone
Progressing deeper into the tissue, advanced SFD leads to muscle and bone invasion, causing severe damage.
Snake fungal lesions may result in necrosis, granulomas, and skeletal impact. This tissue damage complicates treatment, as Ophidiomyces ophiodiicola penetrates beyond the skin, leading to systemic challenges.
Addressing snake fungal pathology early is essential, as untreated infections often lead to irreversible harm in scales and deeper layers.
Invasion of Lungs, Eyes, and Liver
Snake fungal infections can infiltrate critical systems, including lungs (Pulmonary SFD), eyes (Ocular SFD), and liver (Hepatic SFD).
Systemic spread causes pneumonia, internal sores, and respiratory system damage in rare cases.
Ocular SFD leads to cloudy eyes and impaired vision, while hepatic SFD forms liver nodules, risking organ failure.
These severe effects highlight snake fungal disease’s devastating potential without timely intervention.
Disfiguring Facial Lesions
Disfiguring facial lesions mark severe cases of snake fungal disease, leading to significant challenges.
These ophidian skin lesions often cause dramatic changes in appearance, impacting a snake’s ability to hunt or breathe.
Look for:
- Severe swelling or misshapen facial structures.
- Crusty, thickened skin patches or ulcerations.
- Deep nodules that distort natural features.
Lesion severity varies by species, with long-term effects complicating treatment, and can lead to dramatic changes in appearance.
Internal Progression and Pneumonia
As snake fungal disease progresses, the internal spread leads to respiratory complications.
Fungal pneumonia becomes a serious concern, often resulting from lung damage caused by systemic invasion.
Signs include weight loss, lack of appetite, and labored breathing.
These disease symptoms highlight the importance of timely snake fungal diagnosis, as unchecked infections can severely affect essential organs, making recovery increasingly difficult.
Snakes may also exhibit open-mouth breathing, a clear sign of respiratory distress.
Fungal Infection Diagnosis
To confirm a snake fungal infection, you’ll need to rely on a combination of clinical signs and laboratory tests like PCR and histopathology.
These methods identify the fungus responsible and analyze tissue samples, ensuring accurate diagnosis for effective treatment planning.
Laboratory Diagnosis Methods
Diagnosing snake fungal disease involves a mix of lab methods, including culture methods that grow the fungus for identification, while PCR confirmation detects DNA of the Ophidiomyces pathogen.
Histopathology uses lesion biopsy to examine tissue microscopically, revealing fungal invasion. Snake fungal PCR is also available for purchase.
These tools work together to pinpoint the infection, aiding effective treatment. Accurate snake fungal diagnosis hinges on combining these advanced techniques.
PCR and Histopathology Tests
When diagnosing snake fungal disease, PCR tests are a game-changer, offering high accuracy by detecting fungal DNA.
Often paired with histopathology, these methods examine tissue samples but may miss early-stage infections. Contaminated soil contributes to the spread.
Proper sample collection guarantees precise results.
- PCR accuracy is excellent for fungal identification.
- Histopathology limitations include missed subtle infections.
- Sample collection techniques boost diagnostic sensitivity.
Identification of Causative Fungal Pathogen
Pinpointing snake fungal pathogens like Ophidiomyces ophiodiicola involves precise techniques.
Fungal culture helps isolate the pathogen, while DNA detection and PCR confirmation provide accurate results.
Histopathology analysis offers visual proof of Ophidiomyces identification in tissues.
Together, these methods strengthen snake fungal disease diagnosis by identifying the culprit—Ophidiomyces—belonging to Onygenacea.
Accurate identification paves the way for effective monitoring and management strategies.
Clinical Signs and Lesion Patterns
When examining snake fungal disease symptoms, focus on lesion morphology and progression speed.
Look for these signs:
- Scale Abnormalities: Crusty, scabbed, or thickened regions.
- Color Changes: Unusual pigmentation or cloudy spots.
- Behavioral Changes: Unexplained lethargy or abnormal molting.
These dermatological conditions in snakes, including reptile skin lesions and snake fungal scales, can advance, so early detection is key to managing this serious snake skin disorder effectively.
Advanced Disease Symptoms
As the fungal infection advances, you’ll notice severe symptoms like nodules forming deep in the tissues of the head and widespread ulcerations on the skin.
These can lead to systemic complications, including organ damage and a higher risk of disease recurrence or mortality.
Nodules in Deeper Tissues of Head
As snake fungal disease progresses, nodules often form deep in the head’s tissues, particularly around the jaw and skull.
These nodules, composed of infected tissue and fungal buildup, can interfere with movement and feeding.
Diagnostic imaging helps pinpoint nodule location and severity.
Treating these can be tough, as antifungal treatment struggles to penetrate deeper tissues, prolonging recovery.
| Nodule Feature | Example | Effect on Snake | Treatment Challenges |
|---|---|---|---|
| Location | Jaw, skull, head tissues | Impedes feeding | Difficult to reach nodules |
| Composition | Infected tissue, fungus | Swelling and discomfort | Limited medication effectiveness |
| Impact | Restricted mouth movement | Weight loss | Prolonged treatment times |
| Diagnostic Tool | Radiographs, MRI | Targets nodule placement | Requires advanced clinic facilities |
The diagnostic tool used, such as radiographs or MRI, is crucial for understanding the nodule’s impact on the snake’s health.
This information is vital for determining the best course of treatment, which can be challenging due to the location of the nodules.
External Spread and Ulcerations
How does snake fungal disease worsen? External spread can lead to painful ulcerations along the body, neck, and tail, signaling significant tissue damage.
These lesions often invite secondary infections, worsening snake skin disorders.
- Ulceration causes: Poor immune response.
- Spread mechanisms: Environmental fungus exposure.
- Lesion severity: Varies by infection stage.
- Management tips: Consult a snake fungal vet for antifungal treatments and disease management.
Systemic Infections and Organ Damage
As the fungus spreads deeper, it causes systemic issues like organ invasion.
Lung involvement leads to breathing problems, liver damage disrupts vital functions, and eye infections affect vision.
Bone degradation weakens structure, making recovery challenging.
Early snake disease diagnosis is key.
Here’s a glance:
| Symptom | Affected Area | Impact |
|---|---|---|
| Lung Involvement | Lungs | Breathing difficulties |
| Liver Damage | Liver | Reduced organ function |
| Eye Infections | Eyes | Impaired vision |
| Bone Degradation | Skeleton | Weakened structure |
| Systemic Spread | Multiple Organs | Life-threatening effects |
Snake fungal treatment with antifungals and care from a snake fungal vet can limit damage.
Managing systemic progression is tough but essential.
Disease Recurrence and Mortality Rates
When dealing with ophidiomycosis, recurrence factors like improperly sloughed skin and fungal hyphae hiding in tissues can complicate recovery.
Species susceptibility impacts outcomes, with mortality predictors including stress and severe infections.
Though treatment impacts recovery time, recurrence is common.
Long-term effects of snake fungal disease include reduced survival and health, making early intervention critical to protect vulnerable snake species like massasaugas.
Diagnosis involves qPCR and histopathological examination, methods used to detect Ophidiomyces ophidiicola.
Frequently Asked Questions (FAQs)
What are the symptoms of snake fungal disease?
When the chips are down, spotting Snake Fungal Disease involves recognizing crusty skin, cloudy eyes, face swelling, blisters, and ulcers.
These symptoms often vary, but early attention helps manage this troublesome disease effectively, which is a key factor in effective management.
How do you treat a snake fungal infection?
Treating a snake fungal infection involves antifungal medications (topical or systemic), surgical removal of lesions if needed, and supportive care like hydration and temperature control.
Early diagnosis and a veterinarian’s guidance substantially improve recovery chances.
What are the symptoms of a serious fungal infection?
When a fungal infection gets serious, you might notice thickened or crusty skin, painful ulcers, swelling, and even issues like breathing difficulty or cloudy eyes.
Sometimes, it spreads deeper, damaging muscle, bone, or internal organs, which can lead to severe health complications, and even issues like breathing difficulty.
What are the early stages of a fungal infection?
Think of a fungal infection as a slow whisper of trouble—early signs include redness, mild itching, slight swelling, or flaky skin.
You’ll notice subtle changes first, like slight discomfort or tiny, scaly patches forming, which can be a slow whisper of trouble.
How does snake fungal disease affect reproduction?
Snake fungal disease reduces reproduction by weakening affected snakes, limiting their ability to mate or survive long enough to reproduce.
It disrupts ecosystem roles by harming species like Eastern Indigo Snakes, critical for ecological balance, which can be considered a key factor in ecological balance.
What habitat conditions increase the risk of infection?
Moist, warm, and poorly ventilated habitats increase infection risks.
Damp soil, decaying vegetation, or overcrowded areas create ideal conditions for fungal growth, weakening snakes’ immunity.
Regularly inspect and maintain habitats to prevent these environmental triggers.
Can snake fungal disease impact other reptiles?
It’s not just snakes that face the music—other reptiles can be vulnerable too.
Though rare, related fungi have affected species like lizards and turtles.
Environmental exposure and weakened immunity often determine their vulnerability to these fungi.
Are certain snake species immune to SFD?
No snake species is completely immune to Snake Fungal Disease (SFD), but some may show more resistance than others.
Factors like species, habitat, and immune response play roles in how severely they’re affected.
How does the disease affect snake behavior?
The disease can make snakes sluggish, less responsive, and prone to basking longer due to weakened health or discomfort.
You’ll notice changes like reduced hunting, odd hiding habits, and increased vulnerability to predators.
Conclusion
Think of snake fungal infection symptoms as the “check engine” light for your pet—don’t ignore them.
Early signs like scabs, lesions, or molting changes can quickly progress to severe issues, including organ damage and pneumonia.
Acting promptly with proper diagnosis and treatment can make all the difference, and regular monitoring and knowing the progression of these symptoms help protect your snake’s health.
Stay vigilant, and you’ll keep your scaly friend thriving for years to come.
- https://www.cwhc-rcsf.ca/docs/fact_sheets/SFD_FactSheet.pdf
- https://www.gardenwildlifehealth.org/portfolio/snake-fungal-disease/
- https://cwhl.vet.cornell.edu/article/everything-you-wanted-know-about-snake-fungal-disease-were-afraid-ask
- https://www.oriannesociety.org/science-of-scales/snake-fungal-disease-in-georgia/
- https://www.petmd.com/reptile/conditions/parasitic/c_rp_fungal_disease