This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.
This emerging pathogen creates crusty, discolored patches that can spread rapidly across your snake’s body. SFD affects multiple species and can be fatal without proper treatment.
You’ll need veterinary diagnosis through skin samples or PCR testing, as visual symptoms alone can be misleading.
Treatment involves antifungal medications, though success rates vary considerably.
The disease spreads through contaminated environments, making prevention essential through proper hygiene and habitat management. Early detection makes all the difference in treatment outcomes.
Table Of Contents
- Key Takeaways
- Snake Fungal Disease Basics
- Identifying Fungal Infection in Snakes
- Treatment and Management of Fungal Infections
- Prevention and Control of SFD
- Research and Future Directions
- Frequently Asked Questions (FAQs)
- How to treat fungal infections in snakes?
- What does snake fungal disease look like?
- What does a skin infection look like on a snake?
- How does a snake get a fungal infection?
- How do you treat fungal infection in snakes?
- Can humans get snake fungal disease?
- What does fungal infection of the skin look like?
- How common are fungal skin infections in captive snakes?
- Can fungal infections spread from snakes to other reptiles?
- What factors contribute to the development of fungal skin diseases?
- Conclusion
Key Takeaways
- You’ll need professional diagnosis – Visual symptoms alone can’t confirm snake fungal disease, so get PCR testing or skin samples from a vet since other conditions can look similar
- Act fast with antifungal treatment – Early detection makes the biggest difference in recovery outcomes, so don’t wait if you spot crusty lesions, facial swelling, or abnormal shedding
- Focus on prevention through hygiene – Keep enclosures clean, quarantine new snakes for 30 days, and maintain proper humidity levels since the fungus spreads through contaminated soil and surfaces
- Provide supportive care during treatment – Your snake needs proper temperature control, adequate nutrition, and stress reduction alongside antifungal medications to boost immune function and healing
Snake Fungal Disease Basics
Snake fungal disease represents a serious threat to wild snake populations across North America, caused by the environmental fungus Ophidiomyces ophiodiicola that infects snake skin through contaminated soil and surfaces.
Understanding this emerging disease’s basics will help you recognize symptoms early and take appropriate action if you encounter affected snakes in the wild or captivity, which is crucial for the conservation of snake populations and the control of snake fungal disease.
Causes and Transmission of SFD
Understanding snake fungal disease starts with recognizing how Ophidiomyces ophiodiicola spreads through environmental contamination and direct contact.
This pathogen thrives in soil, creating a persistent fungal reservoir that threatens snake populations through various transmission pathways.
Key transmission methods include:
- Soil contamination – The fungus persists in contaminated environments, infecting snakes through habitat exposure
- Direct contact – Snake-to-snake transmission occurs, especially in communal denning sites during winter dormancy
- Environmental spread – Human activities inadvertently track contaminated soil, expanding the pathogen’s geographic reach
The incubation period ranges from 12-37 days after exposure, with environmental stress increasing susceptibility to disease spread.
Symptoms and Clinical Signs of SFD
You’ll recognize SFD through distinctive skin lesions, scabs, and crusty skin that develop across your snake’s body.
Watch for blisters and facial swelling around the eyes and snout, which can progress to severe Facial Disfiguration.
Behavioral Changes include increased basking and lethargy, while Shedding Issues create incomplete molts.
Lesion Severity varies between species, making Diagnostic Challenges common for proper identification.
Impact on Snake Health and Survival
SFD devastates snake health and survival rates substantially. The disease triggers population decline through multiple pathways, causing immune response dysfunction and severe behavioral changes.
Infected snakes experience reproduction impact as facial lesions prevent normal feeding and mating behaviors.
Key health impacts include:
- Reduced hunting ability due to facial disfigurement
- Compromised immune response leading to secondary infections
- Behavioral changes including increased basking and lethargy
- Impaired reproduction affecting snake populations long-term
- Habitat degradation from reduced predator presence
Snake fungal disease creates cascading wildlife health problems throughout ecosystems. Transmission often occurs via contaminated soil transfer.
Species Affected by SFD
Over thirty snake species face snake fungal disease SFD.
Venomous snakes like eastern massasauga rattlesnakes and timber rattlesnakes suffer alongside non-venomous snakes including garter snakes, water snakes, and rat snakes.
Geographic variation exists, with highest impacts in eastern and midwestern regions.
Population decline threatens already vulnerable species, causing significant ecosystem impacts.
The disease is caused by the fungus Ophidiomyces ophiodiicola.
| Snake Family | Example Species |
|---|---|
| Viperids | Timber rattlesnakes, copperheads |
| Colubrids | Garter snakes, black racers |
| Boids | Ball pythons, boas |
| Natricids | Water snakes, ribbon snakes |
Geographic Distribution of SFD
Snake fungal disease spreads across North America and Europe, with confirmed cases in 23 U.S. states and 13 European countries. You’ll find SFD hotspots concentrated in eastern regions, though spread patterns show westward expansion into California.
SFD’s relentless march from eastern strongholds to California threatens snake populations nationwide with devastating efficiency.
The disease, caused by the fungus Ophidiomyces ophidiicola, was first identified in 2006.
Geographic Distribution Highlights:
- North America: Highest prevalence in eastern states, with regional variations showing 54% infection rates in aquatic snakes versus 17% in terrestrial species
- Europe: Confirmed across 13 countries, with Switzerland showing infection hotspots while Spain and Portugal remain unaffected
- Climate Influence: High humidity and 20-30°C temperatures create ideal conditions for future expansion
- Surveillance Gaps: Western states likely underreport cases due to limited monitoring efforts
- Wildlife Impact: Expanding distribution threatens snake populations** through habitat connectivity and environmental changes
Identifying Fungal Infection in Snakes
Recognizing fungal infections in snakes requires careful observation of specific skin changes and behavioral patterns that indicate disease progression.
You’ll need to combine visual inspection with laboratory testing to confirm the diagnosis and distinguish SFD from other skin conditions affecting reptiles, which is crucial for a proper diagnosis.
Visual Signs of Fungal Infection
Early detection proves essential for successful treatment outcomes.
Watch for thickened, crusty skin lesions that appear discolored or scabbed across your snake’s body.
These visual warning signs demand immediate veterinary attention to prevent serious complications.
- Skin lesions with abnormal shedding patterns and crusty textures
- Facial swelling accompanied by cloudy eyes and distorted features
- Nodules ulcerations creating raised bumps under affected skin areas
Laboratory Confirmation of SFD
While visual assessment provides initial clues, laboratory diagnostics confirm your suspicions with scientific certainty.
Fungal culture grows Ophidiomyces ophiodiicola from skin samples, while PCR testing detects fungal DNA with superior diagnostic accuracy.
Histopathology methods reveal tissue changes under microscopy.
However, DNA sequencing through PCR offers the most reliable diagnosis, though sampling technique affects results substantially.
Histopathological Examination and Skin Biopsy
Beyond laboratory tests, histopathological examination through skin biopsy provides definitive diagnosis of fungal infection.
Biopsy techniques collect tissue samples for microscopic analysis, revealing tissue damage patterns and enabling precise fungal identification.
This method offers superior diagnostic accuracy compared to surface swabs, as histopathology examines deeper skin layers where infections establish themselves most effectively.
Environmental factors can also play a significant role in these infections.
PCR and QPCR for SFD Diagnosis
After conducting a biopsy, PCR and qPCR techniques revolutionize Snake fungal disease diagnosis by targeting Ophidiomyces ophiodiicola DNA with remarkable PCR Sensitivity and QPCR Specificity.
These molecular methods detect genetic markers faster than traditional culture approaches, delivering results within hours rather than weeks.
Advanced Assay Development enables Field Applications for wildlife monitoring, making DNA detection accessible for conservation efforts nationwide.
Distinguishing SFD From Other Skin Infections
Properly identifying snake fungal disease requires careful observation, as many conditions mimic SFD’s distinctive appearance.
When examining your snake, focus on specific characteristics that separate fungal infections from other common skin problems.
- Bacterial Infections typically produce wet, oozing lesions with foul odors, unlike SFD’s dry, crusty patches
- Parasitic Infestations cause intense scratching behavior and surface irritation, while snake fungal disease creates deeper nodules
- Thermal Burns and Chemical Exposure leave uniform damage patterns, contrasting with SFD’s irregular, spreading lesions
Professional diagnosis prevents misidentifying Scar Tissue formation as active infection.
Treatment and Management of Fungal Infections
When your snake develops fungal skin infection, you’ll need to act quickly with targeted treatment approaches that address both the infection and underlying health factors.
The treatment process requires careful coordination of antifungal medications, supportive care measures, and environmental management to give your snake the best chance of recovery.
Antifungal Medications and Their Limitations
Antifungal medications face significant obstacles when treating snake fungus.
You’ll encounter drug resistance, where pathogens outsmart terbinafine and itraconazole treatments.
Species variability means what works for rattlesnakes may fail in colubrids.
Systemic antifungals like voriconazole can cause toxicity, while topical antifungals often can’t penetrate deeply enough for efficacy challenges in long-term management.
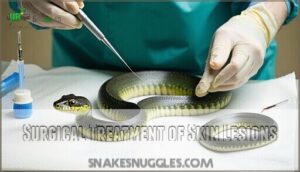
Surgical Treatment of Skin Lesions
Surgical treatment addresses severe fungal lesions through precise excision when antifungal medications prove insufficient.
You’ll find debridement techniques essential for removing infected tissue, while reconstructive surgery may restore damaged areas.
- Lesion excision removes infected tissue completely
- Debridement techniques clean wounds thoroughly
- Grafting options replace severely damaged skin
- Post-operative care prevents secondary infections
- Wound care protocols guarantee proper healing
Thermal, Fluid, and Nutritional Support
Beyond surgical intervention, your snake needs proper thermal regulation, hydration strategies, and nutritional support for recovery.
Maintain ideal temperatures to boost immune function during antifungal treatment snakes require.
Monitor fluid intake carefully, as dehydrated snakes heal poorly. Provide easily digestible foods rich in protein and vitamins.
This supportive care substantially improves recovery outcomes from snake fungal infection, giving your pet the best fighting chance.
Many owners seek specialized snake products during treatment.
Topical and Systemic Antifungal Treatments
With thermal support established, you’ll need targeted medication delivery methods. Topical antifungals applied directly to lesions offer localized treatment, while systemic medications like itraconazole and voriconazole circulate through the bloodstream.
Treatment efficacy varies substantially across species variations, with some snakes showing drug resistance. See a range of antifungal snake products online.
Medication delivery challenges include absorption rates and long-term effects on reptilian physiology.
- Your snake’s recovery depends on choosing the right antifungal treatment snakes protocol
- Snake vet treatment decisions can mean the difference between healing and progression
- Finding effective antifungals feels like searching for a needle in a haystack
- Every failed treatment attempt weighs heavily on both you and your snake’s wellbeing
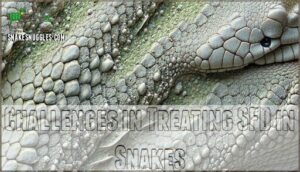
Challenges in Treating SFD in Snakes
Treating snake fungal disease presents significant obstacles.
While antifungal medications offer hope, drug resistance and species variation complicate outcomes.
Treatment stress from handling worsens the infection, creating ethical dilemmas about intervention versus natural processes.
Long-term management remains elusive, as snake vet treatment protocols struggle with:
- Drug resistance developing during extended antifungal treatment courses
- Species variation in response to identical therapeutic approaches
- Treatment stress from frequent handling compromising immune function
- Long-term management requiring months of intensive care with uncertain success
Prevention and Control of SFD
You can substantially reduce SFD transmission risks by implementing proper hygiene protocols and environmental management practices.
Preventing this devastating fungal infection requires understanding how Ophidiomyces ophiodiicola spreads through contaminated soil, surfaces, and direct contact between snakes.
Reducing The Risk of SFD Transmission
You can substantially reduce SFD transmission through proper preventive measures and environmental hygiene practices.
Limit soil tracking by cleaning outdoor equipment before entering snake areas, and always quarantine new snakes for several weeks.
Disinfecting enclosures regularly prevents fungal buildup, while reducing communal denning during winter minimizes contact between infected individuals.
Smart habitat management and consistent cleanliness create barriers against disease prevention failures, ensuring proper preventive measures are in place.
Responsible Handling and Care of Snakes
Safe handling prevents snake skin disease transmission through proper quarantine protocols and habitat maintenance.
You’ll minimize stress by maintaining ideal temperatures, humidity levels, and providing species-appropriate nutritional needs.
Clean enclosures regularly, disinfect tools between animals, and quarantine new snakes for thirty days.
Regular veterinary check-ups are also vital for preventative care.
Watch for snake health issues during routine care.
These snake care tips reduce snake fungal disease risks substantially.
Environmental Factors Contributing to SFD
Beyond proper handling practices, environmental conditions play a significant role in snake fungal disease transmission. Understanding these factors helps you protect both wild and captive snake populations from this emerging threat.
Several environmental conditions create perfect breeding grounds for Ophidiomyces ophiodiicola:
- Soil Contamination – The fungus thrives in contaminated soil and organic matter, persisting for extended periods and creating infection hotspots in snake habitats.
- Habitat Humidity – High humidity levels between 20-30°C provide ideal conditions for fungal growth, making humid environments particularly risky for snake populations.
- Temperature Effects – Warm temperatures combined with moisture create ideal fungal reproduction conditions, while temperature stress weakens snake immune systems.
- Denning Sites – Communal winter denning areas concentrate snakes in contaminated spaces, increasing transmission rates through shared environmental exposure and direct contact.
Human Impact accelerates these problems through habitat destruction, pollution, and climate change, which alter natural environmental conditions and stress snake populations, making them more susceptible to snake fungal disease infections.
Regular habitat disinfection is vital to prevent fungal outbreaks.
Monitoring and Surveillance of SFD
After considering environmental factors, you’ll want to focus on disease monitoring and wildlife surveillance.
Use data collection and strict reporting protocols to track disease prevalence and geographic expansion.
Join citizen science projects or ecological surveillance teams—think of it as being a detective for snakes.
Your careful disease surveillance helps spot outbreaks early, supporting better conservation surveillance and keeping your local snake populations healthier.
Conservation Implications of SFD
Snake fungal disease threatens species conservation through ecosystem impacts and population declines.
When snake populations crash, rodent numbers explode, disrupting food webs.
You can support conservation efforts through these mitigation strategies:
- Report suspected SFD cases to wildlife authorities immediately
- Practice proper habitat preservation by avoiding disturbance during denning seasons
- Support research funding for genetic diversity studies in affected populations
- Advocate for policies protecting snake habitats from development pressures to aid in species conservation.
Research and Future Directions
While researchers have made significant progress understanding SFD, many questions remain about this devastating disease that threatens snake populations across North America.
You’ll find that current studies focus on environmental triggers, stress factors, and developing better treatments to protect these essential predators in our ecosystems.
Understanding The Environmental Factors of SFD
Researchers are piecing together how environmental conditions create perfect storms for Ophidiomyces ophiodiicola outbreaks.
Soil contamination acts as the primary reservoir, while humidity levels above 70% and temperature effects between 68-86°F accelerate fungal growth.
Habitat influence varies dramatically – dense forests with poor air circulation harbor more spores than open areas.
Seasonal variation shows spring emergence from hibernation coincides with peak transmission, when weakened snake populations encounter contaminated soil after months of close contact in communal dens, leading to peak transmission and fungal growth in specific environmental conditions.
Developing Effective Treatments and Preventive Measures
Current breakthroughs in snake fungal care focus on innovative approaches that go beyond traditional antifungal treatment methods.
- Novel Antifungals – Nebulized terbinafine delivers therapeutic levels directly to infected tissue, showing promise where systemic treatments fail in reptile antifungal treatment protocols.
- Probiotic Therapies – Beneficial microorganisms may restore skin flora balance, potentially preventing secondary infections during snake antifungal treatment recovery periods.
- Environmental Remediation – Soil decontamination using targeted disinfection protocols reduces fungal loads in contaminated habitats, supporting snake fungal prevention efforts.
- Immunomodulation Strategies – Thermal support and stress reduction enhance natural immune responses, improving outcomes in reptile fungal care management.
- Genetic Resistance – Research into species-specific susceptibility patterns may identify naturally resistant populations for conservation breeding programs in snake fungal care.
Investigating The Role of Stress Hormones in SFD
Elevated cortisol levels in infected snakes reveal how stress response mechanisms worsen snake fungal disease outcomes.
Stress doesn’t just weaken snakes—it turns their own bodies against them in the fight against fungal invasion.
When you examine captivity effects on wild snakes, hormonal imbalance from confinement amplifies immune suppression, making Ophidiomyces ophiodiicola infections more severe.
Research shows that stressed snakes can’t mount effective defenses against fungal dermatitis, creating a vicious cycle where snake skin disease becomes harder to treat, highlighting the importance of understanding stress response mechanisms.
Comparing Clinical Signs With Laboratory Diagnostics
Laboratory diagnostics often reveal snake skin disease when clinical observation alone falls short.
Visual assessment can miss early-stage ophidian mycosis, making diagnostic accuracy problematic for proper treatment decisions. The spread is exacerbated by contaminated soil.
Effective comparison requires understanding these factors:
- Sign Specificity – External lesions don’t always indicate snake skin fungus severity
- Early Detection – Lab tests identify snake skin infection symptoms before visible signs appear
- Species Variation – Different snakes show varying clinical presentations of diagnosing snake fungus
- Severity Correlation – Laboratory results better predict treatment outcomes than appearance alone
Exploring The Evolutionary Relationships of SFD Susceptibility
Snake species don’t share equal vulnerability to Ophidiomyces ophiodiicola, and understanding species phylogeny reveals fascinating patterns.
Genetic resistance varies across evolutionary history, suggesting adaptation mechanisms influence immune response to fungal pathogens.
This epidemiological puzzle drives researchers to map susceptibility against snake family trees.
| Snake Family | SFD Susceptibility | Evolutionary Advantage |
|---|---|---|
| Viperidae | High vulnerability | Recent pathogen exposure |
| Colubridae | Moderate resistance | Ancient immune adaptations |
| Elapidae | Low infection rates | Specialized defense genes |
| Pythonidae | Variable responses | Geographic isolation factors |
Frequently Asked Questions (FAQs)
How to treat fungal infections in snakes?
Imagine a scaly patient with telltale crusty lesions—you’ll need antifungal medications like itraconazole or voriconazole, plus supportive care including wound management, ideal temperature control, and nutritional support for recovery.
What does snake fungal disease look like?
You’ll notice thickened, crusty skin lesions that look like scabs, along with facial swelling and cloudy eyes. Infected snakes develop abnormal bumps, ulcerated areas, and difficulty shedding properly.
What does a skin infection look like on a snake?
You’ll spot thickened, crusty skin patches, facial swelling, abnormal bumps, and ulcerated areas. Infected snakes develop scabbed lesions, cloudy eyes, difficulty shedding, and distinctive nodules under their skin surface.
How does a snake get a fungal infection?
Environmental exposure transmits fungal infections to snakes.
You’ll find the fungus Ophidiomyces ophiodiicola lurking in contaminated soil, burrows, and organic matter where it survives for extended periods, infecting snakes through direct contact.
How do you treat fungal infection in snakes?
A captive timber rattlesnake in Ohio recovered after receiving antifungal medications and supportive care.
You’ll treat snake fungal disease using antifungals like itraconazole, wound management, and supportive therapy including proper temperature and nutrition.
Can humans get snake fungal disease?
You can’t catch snake fungal disease from infected snakes. This fungal infection, caused by Ophidiomyces ophiodiicola, specifically targets reptile skin and doesn’t transmit to humans through handling or contact.
What does fungal infection of the skin look like?
You’ll see thickened, crusty skin patches that look scabbed or flaky.
Bumps and swellings develop under the skin, especially around the head.
Ulcerated areas appear raw and open, while facial disfiguration becomes noticeable in severe cases, with severe conditions leading to significant changes.
How common are fungal skin infections in captive snakes?
Sure, you’d think your beloved pet snake lives in paradise—but even captive snakes aren’t immune to fungal skin problems.
There have been a number of cases of captive snake populations becoming infected with snake fungal disease.
Can fungal infections spread from snakes to other reptiles?
Yes, fungal infections can spread between reptile species.
Ophidiomyces ophiodiicola, which causes snake fungal disease, has potential to infect lizards, turtles, and crocodiles through contaminated environments, soil, or direct contact with infected animals, showing the potential for contaminated environments to spread disease.
What factors contribute to the development of fungal skin diseases?
High humidity environments, temperatures between 20-30°C, contaminated soil, environmental stress, close contact with infected surfaces, and compromised immune systems create perfect conditions for fungal growth on your reptile’s skin.
Conclusion
Fighting fungal infection in snake skin requires a delicate balance, like walking a tightrope between aggressive treatment and gentle care.
You’ve learned that early detection through proper diagnostic testing, combined with veterinary-prescribed antifungal medications, offers your snake the best chance of recovery.
Remember, prevention through fastidious habitat hygiene, proper humidity control, and stress reduction remains your most powerful weapon against SFD.
Stay vigilant, act quickly when symptoms appear, and maintain consistent environmental standards to protect your serpentine companions, which is crucial for their overall well-being.
- https://www.fws.gov/question-answer/understanding-snake-fungal-disease-impacts-treatments-and-prevention
- https://www.frontiersin.org/journals/fungal-biology/articles/10.3389/ffunb.2023.1064939/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5095536/
- https://pricelab.ca.uky.edu/files/mckenzie_et_al_2021_-_eap.pdf
- https://cwhl.vet.cornell.edu/article/everything-you-wanted-know-about-snake-fungal-disease-were-afraid-ask