This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.
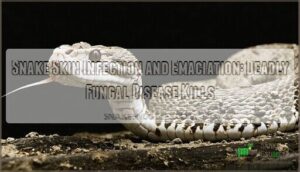
This sneaky fungus creates crusty, mud-like lesions on scales while your snake rapidly loses weight and muscle mass.
Environmental stress, poor husbandry, and weakened immune systems make snakes sitting ducks for this infection.
You’ll spot raised patches, facial swelling, appetite loss, and abnormal shedding patterns.
The disease spreads like wildfire through North American and European snake populations, turning healthy serpents into shadows of their former selves.
Understanding the warning signs can mean the difference between life and death for your scaly friend, and recognizing the impact of Environmental stress and poor husbandry is crucial.
Table Of Contents
- Key Takeaways
- Causes of Snake Skin Infections and Emaciation
- Recognizing Symptoms of Snake Fungal Disease
- Diagnosis and Monitoring of Snake Skin Infections
- Laboratory Methods for Detecting Ophidiomyces Ophiodiicola
- Field Surveillance Techniques for Wild Populations
- Comparing Clinical Signs With Diagnostic Results
- Tracking Disease Progression in Captive Snakes
- Identifying Co-infections and Contributing Pathogens
- Monitoring Stress Hormone Levels in Affected Snakes
- Treatment Approaches for Infected and Emaciated Snakes
- Conservation Strategies for Affected Snake Populations
- Frequently Asked Questions (FAQs)
- What is the early stage of snake blister disease?
- What are the symptoms of snake fungal disease?
- What does a skin infection look like on a snake?
- What is necrotic stomatitis in snakes?
- Can SFD affect other reptiles besides snakes?
- How long can snakes survive with untreated SFD?
- Are certain snake species more resistant to SFD?
- Can SFD recur in snakes after recovery?
- How does climate change impact the spread of SFD?
- Can snake skin infections spread to humans?
- Conclusion
Key Takeaways
- Watch for crusty, mud-like lesions on scales and facial swelling – these are telltale signs of Snake Fungal Disease caused by Ophidiomyces ophiodiicola that can rapidly spread and kill your snake if left untreated.
- Maintain proper environmental conditions to prevent stress – poor humidity, temperature extremes, overcrowding, and habitat fragmentation weaken your snake’s immune system, making it vulnerable to deadly infections.
- Act fast when you notice appetite loss, weight loss, or abnormal shedding – early detection and immediate veterinary treatment with antifungal medications dramatically improve your snake’s chances of survival.
- Practice strict biosecurity measures – quarantine new snakes for 30-90 days, clean equipment with a 10% bleach solution between uses, and avoid handling multiple snakes without proper decontamination to prevent disease spread.
Causes of Snake Skin Infections and Emaciation
You’ll find that snake skin infections and emaciation stem from a complex web of causes that can turn a healthy serpent into a struggling survivor.
From deadly fungal invaders like Ophidiomyces ophiodiicola to environmental stressors and poor nutrition, these factors work together like a perfect storm to compromise your snake’s health.
Ophidiomyces Ophiodiicola Fungus
Ophidiomyces ophiodiicola is an emerging keratinophilic fungus causing Snake Fungal Disease (SFD) across North America and Europe.
This environmental pathogen thrives in diverse conditions, persisting in soil and snake hibernacula.
Multiple species face infection through direct contact or contaminated environments.
The fungus’s genetic adaptability and transmission pathways make it particularly dangerous, with environmental persistence enabling widespread snake skin infections requiring targeted antifungal therapies.
A key symptom of the disease is noticeable facial swelling.
Environmental Factors Contributing to Infections
Environmental stress acts like a perfect storm for snake infections. Habitat fragmentation disrupts natural immunity, while climate change and pollution create ideal breeding grounds for deadly pathogens.
Here’s what weakens your snake’s defenses:
- Habitat Fragmentation – Forces snakes into smaller, overcrowded areas
- Climate Change – Alters temperature and humidity patterns
- Pollution Impact – Contaminates water sources and soil
- Poor Water Quality – Harbors infectious microorganisms
- Degraded Sanitation Standards – Increases pathogen load
These environmental factors compromise immune systems, making snakes sitting ducks for fungal infections.
Stress-induced Susceptibility to Skin Diseases
Multiple stressors wreak havoc on your snake’s immune system, making skin infections nearly inevitable.
Crowded enclosures, frequent handling, and temperature extremes spike cortisol levels like a bad day at work.
Poor nutrition compounds the problem—think of it as running on empty while fighting off germs.
When humidity effects create the perfect storm with these enclosure stressors, your snake’s defenses crumble, opening doors for snake skin infection and emaciation, which can be triggered by temperature extremes.
Parasitic Infestations Affecting Snake Health
Parasitic infestations create a double-whammy for snakes already battling stress.
Mite transmission spreads bacteria while damaging scales, compromising immune function. Internal parasites like ophiotaenia faranciae trigger skin infections and weird behavioral impacts.
You’ll notice infected snakes hiding more, eating less, and looking generally miserable.
Parasite diagnosis requires fecal exams and skin scrapings. Thankfully, treatment options include antiparasitic medications and improved husbandry practices.
Nutritional Deficiencies Leading to Emaciation
Poor nutrition creates a deadly spiral for snakes battling infections.
When you’re dealing with snake emaciation, these nutritional deficiencies weaken their defenses:
- Inadequate prey variety limits essential nutrients
- Vitamin imbalances compromise immune function
- Mineral shortages affect cellular repair
- Husbandry deficiencies prevent proper feeding
Malnourished snakes can’t fight off skin infections effectively, making assisted feeding essential for recovery.
Viral and Bacterial Pathogens in Snake Populations
Bacterial pathogens and viral pathogens silently infiltrate snake populations, creating devastating skin infections and emaciation.
These emerging pathogens exploit weakened immune systems, causing bacterial coinfections that complicate recovery. Viral susceptibility increases when snakes face stress, while antibiotic resistance makes treatment challenging.
The microbiome impact disrupts natural defenses against these microscopic invaders. One such threat is inclusion body disease, which is known to affect boas and pythons.
| Pathogen Type | Common Examples | Primary Effects |
|---|---|---|
| Viral | Serpentovirus, Ferlavirus | Respiratory distress, neurological signs |
| Bacterial | Aeromonas, Pseudomonas | Scale rot, septicemia |
| Co-infections | Multiple pathogens | Rapid decline, high mortality |
| Secondary | Opportunistic bacteria | Complicated viral cases |
| Resistant | Antibiotic-resistant strains | Treatment failures |
Recognizing Symptoms of Snake Fungal Disease
If you’re worried about your snake’s health, spotting the early warning signs of Snake Fungal Disease can be the difference between life and death.
This nasty infection shows up as crusty, thickened skin that looks like someone sprinkled cornflakes on your pet, but it’s no laughing matter when it starts spreading.
Characteristic Skin Lesions and Crusted Scales
Spotting snake skin infection requires careful observation of distinctive warning signs.
You’ll notice these characteristic features that signal trouble ahead:
- Lesion morphology shows raised, irregular patches across the body
- Scale abnormalities create rough, sandpaper-like textures where smooth scales once were
- Crust appearance resembles dried mud or scabs coating affected areas
- Ulcer development creates open wounds with raw, exposed tissue underneath
- Discoloration patterns turn healthy scales into dark, mottled patches
These crusted scales and skin lesions mark snake fungal disease’s unmistakable calling card.
Facial Disfiguration in Affected Snakes
When snake skin infection progresses, facial disfiguration becomes a devastating reality.
Advanced fungal disease creates swollen heads, crusty growths around eyes, and deformed jaw structures that seriously impact feeding and survival.
- Severity Scales help veterinarians assess cosmetic disfigurement levels
- Feeding Impairment occurs when jaw deformities prevent proper prey capture
- Sensory Impact affects vision and smell through facial lesion formation
- Deformity Progression worsens without prompt antifungal treatment intervention
Behavioral Changes Indicating Illness
Watching for telltale behavioral changes can tip you off to snake skin infection before visible symptoms appear.
You’ll notice appetite loss, lethargy signs, and increased hiding behavior as your snake becomes less active.
Activity reduction and erratic movement patterns often signal illness, making these behavioral changes vital early warning signs for detecting problems in your scaly friend.
Progressive Weight Loss and Muscle Wasting
Beyond behavioral shifts, your snake’s body will tell a more alarming story. Progressive weight loss transforms healthy serpents into shadows of themselves.
Watch for these red flags:
- Muscle atrophy making ribs visible through skin
- Anorexia causes leading to complete feeding refusal
- Emaciation stages progressing from slight thinning to skeletal appearance
- Organ failure symptoms like labored breathing
- Nutritional support needs becoming critical
Snake weight loss happens fast with fungal infections. An emaciated snake develops reptile wasting syndrome, where muscle wasting accelerates rapidly.
Think of it like watching ice melt—slow at first, then suddenly everything’s gone. Lethargy and appetite loss can also be early signs of illness.
Sloughing Abnormalities in Infected Snakes
When fungal infections take hold, you’ll notice your snake’s shedding becomes a real mess.
When fungal disease strikes, your snake’s shed turns into a patchy nightmare that won’t come off cleanly
Retained shed clings stubbornly, creating patchy shedding patterns instead of smooth, complete molts.
Scale disruption leads to rough, uneven surfaces, while discoloration causes the skin to look dull or oddly colored.
Shedding frequency increases as the snake struggles with these sloughing abnormalities, making snake skin infection obvious through these telltale signs.
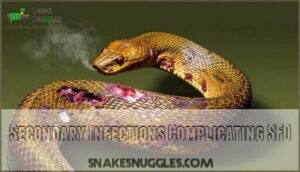
Secondary Infections Complicating SFD
Unfortunately, secondary infections make snake fungal disease even deadlier.
When SFD weakens your snake’s immune system, bacterial involvement creates dangerous complications that can lead to septicemia risk if untreated.
- Bacterial skin infections develop in open wounds, causing putrid odors and tissue damage
- Mite transmission spreads pathogens between scales, worsening fungal synergism throughout the body
- Wound management becomes critical as infected lesions refuse to heal properly
Diagnosis and Monitoring of Snake Skin Infections
You’ll need accurate diagnosis to save infected snakes before the deadly fungal disease spreads through entire populations.
Laboratory tests, field monitoring, and clinical observation work together to catch Snake Fungal Disease early, when treatment still has a fighting chance.
Laboratory Methods for Detecting Ophidiomyces Ophiodiicola
When you spot those crusty scales and facial lesions, you’ll need lab confirmation to nail down the diagnosis.
PCR assays offer the fastest, most sensitive detection of Ophidiomyces ophiodiicola, while culture techniques and histopathology evaluation provide definitive proof.
| Method | Detection Time |
|---|---|
| PCR Assays | 24-48 hours |
| Culture Techniques | 14-25 days |
| Microscopy | Same day |
| Histopathology | 3-5 days |
| Environmental DNA | 24-72 hours |
Field Surveillance Techniques for Wild Populations
While laboratory detection confirms infections, monitoring snake populations in their natural habitats requires different approaches.
Visual surveys remain your primary tool for tracking disease spread across geographic distribution patterns. You’ll spot infected snakes through systematic searches, while eDNA sampling detects fungal DNA in soil and water without capturing animals.
- Visual surveys – systematic searches along transects
- Population monitoring – mark-recapture studies for longterm monitoring
- eDNA sampling – environmental DNA from water sources
- Predictive modeling – mapping disease spread patterns
Comparing Clinical Signs With Diagnostic Results
When you’re tracking down snake skin disease, you’ll need accuracy assessment to match clinical signs with diagnostic results.
Early detection becomes easier when you correlate severity with test outcomes.
PCR tests show high reliability for snake skin lesions, while culture methods face diagnostic challenges with emaciated snake cases.
Predictive modeling helps connect visible symptoms to confirmed snake skin disease diagnosis, using high reliability methods for the best results.
Tracking Disease Progression in Captive Snakes
Your captive snake’s health journey becomes clearer when you monitor lesion tracking and treatment response over weeks. Scientists document how snake skin lesions change, noting if environmental influence affects recovery in your emaciated snake.
This careful observation reveals co-morbidity impact and helps predict long-term outcomes for your snake fungal infection case. A vet may perform skin scraping analysis to identify specific pathogens.
This careful observation reveals co-morbidity impact and helps predict long-term outcomes for your snake fungal infection case.
- Track lesion size, color, and texture changes weekly with photos
- Monitor weight gain and appetite improvements during snake care
- Document environmental factors like humidity and temperature effects
- Schedule regular reptile vet checkups to assess treatment progress
Identifying Co-infections and Contributing Pathogens
Beyond the primary snake fungal infection, you’ll need to uncover bacterial culprits like Pseudomonas that create deadly secondary infections.
Multiple pathogens often work together, causing immune suppression that makes treatment tricky.
| Pathogen Type | Common Species | Impact on Health |
|---|---|---|
| Bacterial culprits | Pseudomonas, Aeromonas | Secondary infections, sepsis |
| Viral pathogens | Paramyxovirus, Adenovirus | Immune suppression, respiratory issues |
| Parasitic infestations | Ophiotaenia, mites | Nutritional deficiencies, skin damage |
| Fungal coinfections | Nannizziopsis | Severe emaciation, treatment resistance |
| Mixed infections | Multiple organisms | Complex symptoms, poor prognosis |
Monitoring Stress Hormone Levels in Affected Snakes
When you’ve identified co-infections, measuring stress hormones becomes your next diagnostic tool.
Cortisol levels reveal how much stress is hammering your snake’s immune system, making recovery harder.
High Cortisol Level Impacts signal Immune Suppression that worsens emaciation and slows healing—especially concerning Captivity Effects on snake health.
Key Stress Biomarkers for Recovery Monitoring:
- Elevated cortisol crushing their fighting spirit against infections
- Chronic stress turning their body into a disease playground
- Weakened defenses letting secondary infections crash the party
- Poor recovery rates breaking your heart as treatments fail
Treatment Approaches for Infected and Emaciated Snakes
When your snake shows signs of fungal infection or severe weight loss, quick action can mean the difference between recovery and death.
Treatment combines targeted antifungal medications with careful supportive care to help these reptiles regain their strength and fight off disease.
Antifungal Therapies for Snake Fungal Disease
Once you’ve identified the infection, antifungal therapies become your main defense against Snake Fungal Disease.
Topical treatments like clotrimazole target localized lesions, while systemic antifungals such as terbinafine and voriconazole fight widespread infections.
Surgical intervention may remove severe lesions.
If you’re looking for effective antifungal products, several options are available.
These treatment efficacy rates vary by species, but early action improves outcomes substantially.
Supportive Care for Emaciated Individuals
While antifungal medications target the infection, emaciated snakes require thorough supportive care to survive.
Thermal support maintains body temperature, while fluid therapy prevents dehydration. Stress reduction through quiet environments aids recovery.
Assisted feeding may help, but veterinary care determines timing. Vitamin supplementation addresses nutritional deficiencies underlying the emaciation.
Regular check-ups can help with early detection of illness.
Addressing Underlying Nutritional Deficiencies
When dealing with emaciated snakes, you’ll need to tackle nutritional deficiencies head-on. These gaps in snake nutrition can worsen existing health problems and slow recovery.
Here’s your action plan:
- Diet Assessment – Review current feeding schedules and prey types
- Supplementation Strategies – Add essential vitamins targeting specific imbalances
- Assisted Feeding – Help severely weakened snakes consume nutrition
- Hydration Importance – Make certain adequate fluid intake during supportive care
Consider using snake vitamin supplements to address these deficiencies.
Managing Environmental Factors to Reduce Stress
Beyond nutrition, you’ll need to tackle environmental factors that spike snake stress. Think of it as creating a snake spa – your patient needs perfect conditions to heal.
Temperature gradients matter most. Set up warm and cool zones so your snake can thermoregulate naturally. Humidity control prevents respiratory issues while supporting healthy shedding. Enclosure size should allow natural movement without feeling exposed.
| Environmental Factor | Ideal Range | Stress Indicators |
|---|---|---|
| Temperature | Species-specific gradient | Lethargy, poor appetite |
| Humidity | 50-80% depending on species | Stuck shed, respiratory issues |
| Light cycles | 12-hour day/night cycle | Disrupted feeding patterns |
Hiding places are non-negotiable – stressed snakes won’t eat or heal properly. Create multiple snake habitats within the enclosure using natural materials. The snake environment should feel secure, not like a fishbowl.
Many keepers find success using a proper temperature gradient to keep their snakes healthy. Habitat restoration principles apply even in captivity. Minimize vibrations, reduce handling, and maintain consistent conditions.
When environmental factors align with natural needs, your snake’s immune system gets back on track.
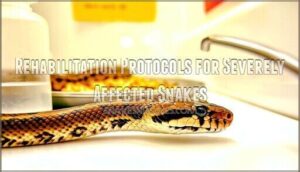
Rehabilitation Protocols for Severely Affected Snakes
Severely affected snakes require intensive wound management and quarantine procedures to prevent reinfection.
You’ll implement assisted feeding protocols when appetite returns, ensuring proper medication delivery through oral or topical routes.
Supportive care addresses nutritional deficiencies with vitamin supplements while antifungal therapies continue.
Long-term monitoring tracks healing progress, with snake recovery depending on consistent environmental controls and patient treatment approaches.
Evaluating Treatment Efficacy and Recovery Rates
After implementing rehabilitation protocols, tracking treatment outcomes becomes your roadmap to success.
Recovery rates vary dramatically – captive snakes show substantial improvement with combined antifungal treatment and supportive care, while wild populations face grimmer prospects.
Monitoring signs like restored feeding, normal shedding, and weight gain indicates progress.
However, recovery timeline extends months, requiring patience.
Relapse prevention demands ongoing vigilance since long-term effects can resurface unexpectedly.
Conservation Strategies for Affected Snake Populations
You’ll need to act fast when Snake Fungal Disease hits your local snake populations—conservation efforts can make the difference between species survival and local extinction.
Protecting these reptiles requires a multi-pronged approach that combines habitat management, public awareness, and scientific collaboration to give infected populations their best shot at recovery.
Habitat Restoration to Promote Snake Health
Beyond treatment, you’ll need to tackle the root problem: degraded habitats.
Healthy environments naturally boost snake immunity and reduce infection risks. Native vegetation provides better shelter and prey, while invasive removal eliminates disease vectors. Clean water sources prevent dehydration, and connectivity corridors let snakes escape contaminated areas.
- Native plants create bug buffets – more insects mean healthier, well-fed snakes
- Clean streams wash away fungal spores that cause deadly skin infections
- Connected habitats offer escape routes from contaminated areas during outbreaks
- Diverse ecosystems build stronger immune systems through varied prey and reduced stress
Public Education on Snake Fungal Disease
Three simple steps can turn you into a snake fungal disease awareness champion.
First, share snake fungal disease symptoms with hiking groups—crusty scales and facial swelling are red flags.
Second, teach responsible handling techniques to prevent disease spread.
Finally, support citizen science projects that track SFD outbreaks.
Your public education efforts protect entire populations through biosecurity education.
Implementing Biosecurity Measures in Snake Habitats
Protecting snake populations requires strategic biosecurity measures that act like invisible shields against fungal invaders.
You can’t just hope for the best when snake fungal disease threatens entire ecosystems.
Effective habitat protection starts with these Disease Prevention fundamentals:
- Quarantine Protocols – Isolate new or sick snakes for 30-90 days before habitat introduction
- Decontamination Methods – Clean equipment with 10% bleach solution between different snake areas
- Monitoring Effectiveness – Track infection rates through regular visual surveys and environmental DNA sampling
Smart biosecurity transforms environmental factors from disease highways into protective barriers, giving your conservation efforts real teeth against this deadly threat.
Captive Breeding Programs for Vulnerable Species
Captive breeding programs serve as genetic diversity insurance for vulnerable snakes facing health crises.
You’ll see facilities producing 200 Louisiana pinesnake hatchlings yearly, while Florida’s eastern indigo program releases 20-30 snakes annually.
These reintroduction strategies combat nutritional deficiencies and snake health problems through careful snake treatment protocols.
Program sustainability depends on habitat availability and monitoring survival rates of 58-75% post-release.
Collaborative Research Initiatives on Snake Health
Scientists are teaming up like never before to fight snake health problems.
Global partnerships share critical data sharing on snake fungal disease research, while interdisciplinary teams combine veterinary medicine with ecology.
Standardized protocols help researchers compare results across continents.
These research initiatives pool funding models and expertise, creating powerful networks that tackle snake health challenges faster than any single lab could manage alone.
Regular checkups can aid in early symptom detection.
Long-term Monitoring of Population Dynamics Post-infection
When monitoring snake populations after fungal disease outbreaks, you’re tracking nature’s recovery story.
Population dynamics reveal how snake survival rates, genetic diversity, and ecosystem impacts evolve over time.
These adaptation strategies help identify which populations develop disease resistance.
Long-term data shows whether snake conservation efforts actually work, guiding future protection plans for vulnerable species, and informing how to improve disease resistance.
Frequently Asked Questions (FAQs)
What is the early stage of snake blister disease?
Roughly 80% of snake blister disease cases start with small, clear fluid-filled bumps on your snake’s belly scales.
You’ll notice these sterile blisters before bacterial infection sets in, making early detection essential for treatment success.
What are the symptoms of snake fungal disease?
You’ll notice crusty, thickened skin lesions and facial disfiguration that look like fungal growth. Your snake might hide more, eat less, and develop abnormal shedding patterns or cloudy eyes.
What does a skin infection look like on a snake?
Like a battlefield scar telling its story, snake skin infections reveal themselves through crusty, thickened patches, ulcerated scales, abnormal bumps, and discolored areas that look angry and inflamed.
What is necrotic stomatitis in snakes?
Necrotic stomatitis, or "mouth rot," causes infected gums, teeth, and mouth tissues to die and decay. You’ll see yellowish pus, swollen gums, and foul odor around your snake’s mouth area.
Can SFD affect other reptiles besides snakes?
Currently, SFD primarily affects snakes, but you’ll occasionally see it in other reptiles like lizards.
The Ophidiomyces fungus seems to prefer snake hosts, though researchers are still studying its full range across different reptile species.
How long can snakes survive with untreated SFD?
Survival time varies widely – some snakes die within months while others can live years with SFD, depending on disease severity, species, and overall health. Early intervention dramatically improves outcomes.
Are certain snake species more resistant to SFD?
Some species dodge SFD better than others—it’s nature’s unfair lottery system.
You’ll find eastern species like timber rattlesnakes get hit harder, while western snakes often show more resistance to infection.
Can SFD recur in snakes after recovery?
Yes, SFD can definitely come back after you think your snake’s recovered.
The fungus likes to stick around in the environment, and stressed or weakened snakes become vulnerable again.
It’s frustrating, but proper husbandry helps prevent reinfection.
How does climate change impact the spread of SFD?
Climate change creates perfect storm conditions for SFD spread.
You’ll see warmer temperatures and shifting weather patterns stress snake immune systems, making them sitting ducks for infections.
Meanwhile, habitat changes force snakes into closer contact, accelerating disease transmission.
Can snake skin infections spread to humans?
Generally, snake skin infections won’t jump to humans, but you should still wash your hands after handling infected snakes.
Some bacteria can occasionally cause minor skin irritation if you’ve got cuts, which is a key reason to practice good hygiene.
Conclusion
Protecting your snake from the devastating effects of snake skin infection and emaciation starts with understanding that prevention beats treatment every time.
You’ve learned that Ophidiomyces ophiodiicola doesn’t discriminate—it’ll attack any stressed, weakened serpent given the chance.
Your best defense is to maintain proper humidity, quarantine new arrivals, and watch for those telltale crusty lesions.
Early detection saves lives, so don’t ignore subtle changes in appetite or behavior, and with vigilant care and quick veterinary intervention, you can help your scaly companion beat this deadly fungal menace.
- https://www.ingleside.com/services/other-pets/blog/skin-and-shell-infections-reptiles-causes-symptoms-and-treatment
- https://www.merckvetmanual.com/exotic-and-laboratory-animals/reptiles/bacterial-diseases-of-reptiles
- https://royalsocietypublishing.org/doi/10.1098/rstb.2015.0457
- https://www.petmd.com/reptile/care/evr_rp_how-can-i-tell-if-my-snake-sick
- https://www.vetlexicon.com/exotis/reptiles/nutrition/articles/anorexia/