This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.

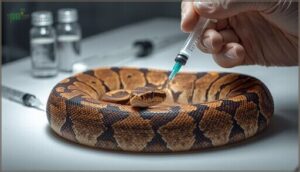
Your snake’s life depends on milligrams—not guesswork, not folklore, not “what worked for my friend’s python.” A single miscalculated dose of aminoglycosides can trigger irreversible renal failure. Too little fenbendazole, and those nematodes survive to reproduce.
Veterinary herpetology operates in precise ranges: 5 mg/kg versus 10 mg/kg isn’t a minor difference—it’s the gap between therapeutic success and organ toxicity.
This dosage guide translates complex pharmacology into concrete protocols you can execute safely. You’ll learn exact calculations for antibiotics, antifungals, antiparasitics, and supportive medications, plus administration techniques that minimize stress while maximizing bioavailability.
Table Of Contents
- Key Takeaways
- Safe Antibiotics for Snakes
- Antifungal and Antiviral Medications
- Parasite Treatments and Dosage
- Supportive Medications and Supplements
- Best Practices for Medication Administration
- Frequently Asked Questions (FAQs)
- Are there drugs available for anesthesia in snakes?
- What is the best steroid for snakes & lizards?
- Does metronidazole kill snakes?
- Can a snake be injected into a syringe?
- Should nephrotoxic drugs be given to sick reptiles?
- What medications are safe for gravid snakes?
- Can medications impact a snakes shedding process?
- Are there safe medications for dehydrated snakes?
- How to store medications for snake use?
- Are herbal remedies safe for snake treatment?
- Conclusion
Key Takeaways
- Snake medication dosing operates in precise mg/kg ranges where the difference between 5 mg/kg and 10 mg/kg can mean therapeutic success versus organ toxicity, making exact weight-based calculations and species-specific protocols non-negotiable for safety.
- Aminoglycosides like amikacin carry nephrotoxicity risks that demand strict hydration monitoring, while fluoroquinolones risk tissue necrosis at injection sites—both require veterinary oversight and careful adverse reaction tracking within 24–72 hours post-administration.
- Antiparasitic treatments follow specific regimens (fenbendazole 50 mg/kg daily for 3–5 days, praziquantel 5–10 mg/kg single dose) with mandatory follow-up testing 2–4 weeks later to confirm parasite clearance and prevent resistance from incomplete protocols.
- Documentation of every dose—drug name, concentration, route, time, observed response—creates the data trail essential for adjusting protocols, tracking treatment milestones, and preventing the medication errors that compromise snake survival in clinical practice.
Safe Antibiotics for Snakes
Bacterial infections in snakes require targeted antibiotic therapy, with efficacy and safety margins determined by species, weight, and administration route. Your veterinarian will select from aminoglycosides, fluoroquinolones, cephalosporins, penicillins based on culture results, infection site, and individual tolerance.
Proper diagnosis through bacterial culture and sensitivity testing is essential, so consult a reptile veterinarian to determine which antibiotics work best for your snake’s specific infection.
Below are commonly prescribed antibiotics, precise dosing protocols, and species-specific considerations for corn snakes, gopher snakes, tortoises, and most colubrid species.
Commonly Used Antibiotics
Bacterial infections demand swift intervention—antibiotic resistance won’t wait. You’ll rely on three proven agents:
- Aminoglycosides: Amikacin, gentamicin—nephrotoxic, maintain hydration strictly
- Fluoroquinolones: Enrofloxacin, ciprofloxacin—tissue necrosis risk at injection sites
- Macrolides: Azithromycin—respiratory spectrum, limited reptile data
Medication safety hinges on species-specific dosage calculations. Snake health deteriorates rapidly with incorrect protocols—precision mandatory, guesswork contraindicated.
Dosage Recommendations by Species
You’ll calculate every dose per kilogram—precision prevents toxicity. Enrofloxacin: 5–10 mg/kg IM or PO daily; colubrids tolerate higher ranges, viperids require conservative titration. Amikacin: species-specific nephrotoxicity thresholds demand careful escalation.
Calculate every antibiotic dose per kilogram—precision prevents toxicity, and species-specific thresholds demand careful titration
Ampicillin: 10–20 mg/kg SC/IM every 12 hours most species, tortoises need 50 mg/kg. Ceftazidime: 20–40 mg/kg SC/IM/IV every 2–3 days.
Reptile pharmacology isn’t one-size-fits-all—your snake’s taxonomy dictates safe veterinary guidelines and dosing protocols. For best outcomes, always base medication on accurate animal weight measurement.
Monitoring for Adverse Reactions
Once you’ve dosed your snake, watch for appetite shifts within 24 hours—refusal signals intolerance. Hydration checks every 6–12 hours are essential: assess skin turgor and mucous membranes. Behavior tracking is crucial to capture signs of lethargy or restlessness—deviations from the baseline matter.
Daily weight fluctuations during the first week can reveal hidden toxicology issues. Document drug therapy carefully, noting the drug, dose, route, time, and response. Reptile medicine demands vigilant reassessment—adverse reactions in snakes don’t always announce themselves loudly.
Antifungal and Antiviral Medications
Fungal and viral infections require targeted therapy—delayed treatment compromises outcomes. Antifungals address dermatophytes, aspergillosis, systemic mycoses; antivirals target herpesvirus, paramyxovirus, inclusion body disease.
Identifying skin lesions early helps veterinarians choose the right antifungal or antiviral protocol, and this guide to skin lesions in pet snakes walks through common presentations and diagnostic steps.
Dosing protocols vary markedly across snake species, demanding precise calculation and route selection.
Approved Antifungal Drugs and Doses
Fungal infections in snakes require prompt, species-specific antifungal treatment. Amphotericin B (0.5–1 mg/kg intracoelomic q 1–3 d) is effective against Aspergillosis, while itraconazole (5–10 mg/kg PO q 1–2 d) offers broad-spectrum coverage for molds. Fluconazole (5 mg/kg PO q 24 h) is used to manage systemic candidiasis. Ketoconazole is rarely utilized due to its hepatotoxicity risk. It is essential to monitor liver enzymes, watch for drug resistance, and document treatment outcomes to ensure medication safety and optimized dosing.
Here is a list of antifungal treatments and their applications:
- Amphotericin B – 0.5–1 mg/kg intracoelomic, IV q 1–3 d for Aspergillosis, 14–28 d course
- Itraconazole – 5–10 mg/kg PO q 1–2 d, broad antifungal coverage, chameleons
- Fluconazole – 5 mg/kg PO q 24 h lizards; 21 mg/kg SC then 10 mg/kg 5 d later, sea turtles
- Clotrimazole – Topical application for fungal dermatitis, minimal systemic absorption
- Hepatic monitoring – Serial liver enzyme checks during prolonged azole or polyene therapy
Antiviral Options and Usage Guidelines
You’ll find limited antiviral medications approved for reptile health, though acyclovir (80 mg/kg PO q 8 h or 240 mg/kg q 24 h) targets certain viral infections.
Antimicrobial therapy for infectious disease management requires strict medication adherence and dosing strategies customized to viral load management.
Treatment outcomes depend on early intervention; antiviral resistance emerges when protocols lapse, so you must document each dose rigorously.
Application Methods and Safety Tips
Administration routes demand precision—oral, intramuscular, topical—matched to reptile formulary specifications and medication interactions risk profiles.
- Secure calm restraint during injections, aseptic technique prevents infection
- Dilute concentrates exactly per label, prevents irritation or dosing errors
- Topical applications: specified area only, avoid mucous membranes completely
- Observe 24–72 hours post-dose for vomiting, lethargy, respiratory changes; seek veterinary intervention immediately if adverse reactions occur
Parasite Treatments and Dosage
Parasites are some of the most common health challenges you’ll face with captive snakes, from nematodes in the gut to lungworms in the respiratory tract.
Treatment requires precision—wrong dosages or missed follow-ups can leave infestations unchecked or harm your snake. Here’s what works, how much to give, and when to repeat.
Effective Antiparasitic Medications
Praziquantel eliminates tapeworms at a single dose of 5–10 mg/kg. Fenbendazole targets nematodes with 50 mg/kg daily for 3–5 days. Albendazole is used for gastrointestinal parasites, administered at 5–10 mg/kg every 5–7 days, up to three doses. Ivermectin treats ectoparasites at 0.2 mg/kg once, with close monitoring for neurologic toxicity. Mebendazole is effective against intestinal worms, given at 100 mg/kg divided over 3 days.
Species-specific metabolism dictates antiparasitic drug selection, and parasitology confirms treatment options for ideal snake health and medication safety in parasite control.
Step-by-Step Dosage Instructions
Weigh your snake to the nearest gram—dose calculation hinges on precise body mass. Multiply weight in kg by the prescribed mg/kg dose. Divide by drug concentration (mg/mL) to determine injection volume.
For oral medications, mix with water or saline. Administer subcutaneously or orally per protocol. Document time, route, volume.
Medication safety demands exact measurement; treatment schedules prevent under- or overdosing in reptile care and management. For additional context on proper procedures, review these dosage instructions in healthcare.
Repeat Treatments and Follow-Up Care
If stool tests stay positive after your initial antiparasitic course, you’ll need repeat reptile care within 7–14 days under veterinary direction. Schedule follow-up visits 2–4 weeks post-treatment to verify parasite clearance through lab work and symptom monitoring.
Document appetite, activity, and stool changes daily—your home care tips build recovery planning. Clean enclosures weekly to prevent reinfection; proper animal health care and reptile disease treatment demand both medication and environmental control.
Supportive Medications and Supplements
Beyond treating infections and parasites, your snake may need supportive care to recover from illness, surgery, or environmental stress.
Fluids, vitamins, and adjunct therapies stabilize critical patients and accelerate healing when primary medications alone aren’t enough.
Here’s what you need to know about safe supplementation and supportive protocols.
Safe Use of Fluids and Electrolytes
You’ll stabilize critical snakes with isotonic crystalloids—lactated Ringer’s or normal saline at 15–25 ml/kg, SC or ICe, q 24 h. Fluid balance demands precise weight tracking, urine output assessment, and skin turgor checks.
Electrolyte management requires serial labs every 4–6 h during resuscitation techniques; correct sodium deficits gradually (≤8–12 mEq/L per 24 h), potassium with ECG monitoring.
Hydration monitoring through mucous membrane moisture and capillary refill guides IV fluids adjustments in reptile anesthesia, veterinary care contexts for ideal reptile care, and animal health outcomes in reptiles.
Vitamin and Mineral Supplementation
Beyond electrolyte rescue, you’ll address vitamin needs and mineral deficits in compromised snakes. Calcium gluconate: 300 mg/kg, IM or ICe, corrects hypocalcemia; injectable vitamin A: 1,000–5,000 IU/kg, IM, once, reverses ocular and integument pathology. Monitor supplement safety—excess fat-soluble vitamins accumulate. Nutrient interactions matter:
- Calcium absorption requires vitamin D₃ co-administration
- Iron interferes with phosphorus metabolism
- Dietary balance trumps isolated dosing for reptile nutrition, animal health outcomes in veterinary medicine, reptile care protocols
Adjunct Therapies for Recovery
Adjunct therapies accelerate convalescence when primary medications alone plateau.
Physical therapy—gentle range-of-motion exercises three times weekly—restores mobility post-trauma. Butorphanol: 0.5–2 mg/kg, IM, q 12–24 h, provides pain relief during wound healing.
Behavioral support via stress reduction, dim lighting, minimizes cortisol spikes.
Nutritional care: high-protein prey items every 5–7 d sustain anabolic recovery under anesthesia and analgesia protocols.
Best Practices for Medication Administration
You’ve got the right medications—now you need the right execution. Dosage errors, poor technique, incomplete records: each puts your snake at risk.
Here’s how to administer treatments safely, track responses accurately, and avoid the mistakes that compromise therapy.
Calculating Accurate Dosages
You’ll prevent most medication errors by mastering three checkpoints: accurate weight conversion to kilograms, verification of medication concentration on the vial, and dose calculation using the prescribed mg/kg.
For snakes, species pharmacokinetics demand conservative pediatric dosing in neonates—amikacin and similar drug dosages illustrate how anesthesia and analgesia protocols hinge on careful pharmacology.
Always double-check your math before administering.
Safe Injection and Oral Techniques
Once you’ve calculated your dose, technique determines success. Intramuscular injections—amikacin, ketamine, medetomidine—go mid-body, cranial third; you’ll avoid nerve bundles there. Subcutaneous routes work for fluids behind paraspinal folds. Oral administration demands firm, gentle restraint: aim toward the back of the tongue using calibrated syringes for dosing accuracy.
- New sterile needle for each patient prevents cross-contamination
- Warm anesthetic agents to room temperature before injection
- Monitor injection sites within 24 hours for swelling or discharge
Record-Keeping and Ongoing Assessment
Documentation anchors every clinical decision you make. Log species, dose, route, time, observed response—each entry becomes data for outcome tracking.
Daily weight, appetite, lesion progression: monitor systematically. Schedule reassessments at fixed intervals; treatment milestones guide dose adjustments.
Secure medical record security with audit trails, role-based access. Retain records seven years minimum.
Quality improves when follow-up schedules and data analysis inform your next protocol.
Frequently Asked Questions (FAQs)
Are there drugs available for anesthesia in snakes?
Anesthesia Options exist—you won’t be left in the dark. Injectable agents like ketamine, medetomidine, and alfaxalone provide snake sedation.
Inhalant anesthetics such as isoflurane maintain anesthesia with proper airway management and pain relief protocols.
What is the best steroid for snakes & lizards?
No single steroid suits all reptiles. Prednisolone treatment (1–5 mg/kg PO) is often preferred for snakes and lizards with immune-mediated inflammation.
Dexamethasone effects include potent immunosuppression, reserved for severe shock under strict veterinary pharmacology guidance.
Does metronidazole kill snakes?
Metronidazole, when dosed correctly at 20–50 mg/kg every 24–48 hours, won’t kill snakes. However, overdose causes metronidazole toxicity, leading to neurological signs and ataxia.
Always confirm the diagnosis, calculate the dose precisely, and monitor closely. Veterinary guidance is essential to prevent snake health risks.
Can a snake be injected into a syringe?
No—medicine is drawn into a syringe, then administered to your snake. Injection techniques require veterinary guidance to avoid medication errors.
Proper syringe safety and snake handling prevent tissue damage during antimicrobial delivery.
Should nephrotoxic drugs be given to sick reptiles?
Nephrotoxic drugs carry significant kidney function risks in reptiles.
Your veterinarian weighs benefits against renal health monitoring needs, often choosing safer antibiotics or adjusting doses when kidney reserve is uncertain or compromised.
What medications are safe for gravid snakes?
Picture a coiled gravid female, eggs developing: pregnancy safety demands caution. Enrofloxacin 5 mg/kg, ceftazidime 20 mg/kg divided, fluconazole 10 mg/kg—antimicrobial drugs and reptile pharmacology intersect.
Wildlife medicine prioritizes gravid care, minimizing medication risks in zoological medicine contexts.
Can medications impact a snakes shedding process?
Yes. Antibiotics, antifungals, diuretics alter hydration levels and skin health. Dehydration causes incomplete sheds. Stress from handling and osmotic imbalance delays shedding cycles.
Monitor humidity, eye caps, and retained shed during treatment. Consult a herpetology specialist immediately.
Are there safe medications for dehydrated snakes?
Subcutaneous fluids, lactated ringers 15–25 ml/kg q 24 hr, administered under veterinary supervision, rehydrate effectively. Oral electrolyte solutions support hydration. Emergency treatment requires immediate fluid therapy, species-specific protocols, ongoing assessment.
How to store medications for snake use?
Store antibiotics, antifungals in cool, dry locations—60–77°F—away from light, moisture. Use original containers, opaque bottles for photosensitive drugs. Label clearly, rotate stock by expiration, refrigerate biologics only per veterinary direction.
Are herbal remedies safe for snake treatment?
Walking a tightrope without a net—herbal remedies for snakes carry unpredictable risks. Plant toxicity, variable snake species responses, herbal interaction effects, and absent herpetological research make natural remedy alternatives unreliable compared to evidence-based reptile care.
Conclusion
An ounce of prevention beats a pound of cure”—especially when that cure involves nephrotoxic antibiotics. You now possess the framework for evidence-based intervention: precise mg/kg calculations, species-appropriate protocols, adverse reaction monitoring.
This safe medications for snakes dosage guide bridges textbook pharmacology and cage-side reality. But remember—veterinary consultation remains non-negotiable. Your snake’s physiology doesn’t forgive approximations. Measure twice, dose once, document everything. Their survival depends on your clinical precision.
- http://www.iwrc-online.org/
- http://www.mlanet.org/resources/medspeak/medshort.html
- https://www.furrycritter.com/pages/pharma/reptiles/methylprednisolone.htm
- https://www.msdvetmanual.com/pharmacology/inflammation/corticosteroids-in-animals
- https://ratguide.com/meds/endocrine_hormones/glucocorticoids/prednisone_prednisolone.php