This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.
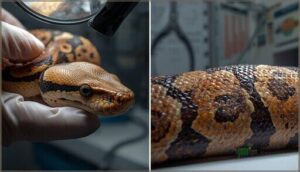
A snake’s skin isn’t just armor—it’s a diagnostic map that reveals when something’s gone wrong beneath the surface. When bacterial agents like Pseudomonas colonize moisture-trapped scales, or when Ophidiomyces ophidiicola etches its telltale crusted lesions across the integument, you’re looking at infections that can progress from localized dermatitis to systemic compromise within days.
The challenge lies in distinguishing normal shedding irregularities from pathogenic invasion, because by the time foul-smelling discharge appears or blisters erupt between scales, secondary complications may already be underway.
Recognizing snake skin infections early demands attention to subtle clinical markers—the slight erythema at scale margins, the unexpected edema, the distinct boundary where healthy tissue meets compromised dermis. Understanding these diagnostic clues and their underlying causes gives you the framework to act decisively before treatable dermatological conditions escalate into complex medical emergencies.
Table Of Contents
Key Takeaways
- Snake skin infections progress rapidly from localized dermatitis to systemic disease, making early recognition of subtle markers like scale margin erythema, unexpected edema, and distinct boundaries between healthy and compromised tissue essential for preventing medical emergencies.
- Most skin infections stem from preventable husbandry failures—poor hygiene, excessive humidity above 70–80%, traumatic injury, and ectoparasite infestation—rather than inevitable pathogen exposure, meaning proper environmental control directly reduces infection risk.
- Accurate diagnosis requires distinguishing infection from normal shedding, trauma, and genetic disorders through systematic physical examination, skin scraping, fungal cultures, and advanced imaging, as visual assessment alone won’t differentiate bacterial, fungal, viral, or parasitic causes.
- Effective treatment demands both targeted medications (third-generation cephalosporins for resistant bacteria, itraconazole or voriconazole for deep fungal infections) and correcting the underlying environmental deficiencies, with recovery taking three weeks to several months depending on infection severity and treatment compliance.
What Are Snake Skin Infections?
Snake skin infections represent a spectrum of cutaneous diseases caused by bacterial, fungal, viral, and parasitic pathogens that compromise the integumentary barrier.
These conditions arise from complex interactions between environmental stressors, suboptimal husbandry practices, and opportunistic microorganisms that exploit your snake’s weakened defenses.
Grasping the basic causes and types of infectious agents will help you recognize early warning signs and seek appropriate veterinary intervention before minor issues progress to life-threatening systemic disease.
Definition and Overview
Snake skin infections represent pathological processes affecting the integument, scales, or underlying soft tissues—and they’re more common than you might think. Dermatologic disease accounts for roughly 13–24% of clinical presentations in pet reptiles.
You’ll encounter four main infection pathogens:
- Bacterial agents causing ulcerative dermatitis or “scale rot”
- Fungal diseases like ophidiomycosis targeting keratin layers
- Viral infections producing characteristic blistering
- Parasitic conditions manifesting as localized skin lesions
Understanding these categories helps you recognize what’s normal versus concerning. Reptile owners should be aware of reptile bacterial diseases to provide proper care.
Common Causes in Snakes
While infections arise from bacterial, fungal, viral, or parasitic agents, most cases stem from preventable husbandry failures. Poor hygiene—accumulated feces, soiled substrates—creates a breeding ground for opportunistic pathogens. Excessive moisture above 70–80% humidity macerates ventral scales, allowing entry for bacteria and fungi. Traumatic injury from rough furnishings compromises skin integrity. Ectoparasite infestation with snake mites disrupts the barrier. Even nutritional deficiency weakens immune defenses, making your snake vulnerable.
Recognizing these signs is vital for addressing snake skin problems and ensuring proper care.
Types of Infectious Agents (Bacterial, Fungal, Viral, Parasitic)
Understanding the infectious agents behind skin disease helps you target treatment effectively. Four major pathogen groups drive most cases:
- Bacterial infections: Gram-negative rods like Pseudomonas and Aeromonas cause purulent ulcers and septicemia
- Fungal diseases: Ophidiomyces ophidiicola produces crusted, erosive lesions in ophidiomycosis
- Viral outbreaks: Poxviruses and iridoviruses trigger nodular plaques
- Parasitic infections: Mites and ticks damage scales, enabling secondary invasion
Skin microbiology reveals how these agents interact, often as co-infections.
Key Signs of Snake Skin Infections
Spotting a skin infection early can make all the difference in your snake’s recovery. You’ll want to know what separates a minor issue from something that needs immediate veterinary attention.
Here are the four key signs that should raise your concern.
Redness, Swelling, and Blistering
When you first notice your snake’s scales turning red and puffy, you’re witnessing the body’s alarm system in full swing. These infection symptoms—particularly blister formation and edema—often signal bacterial or fungal dermatitis taking hold. In one clinical survey, experimental fungal infections produced localized swelling in 100% of snakes, while bacterial outbreaks triggered widespread skin lesions across entire body surfaces.
| Clinical Sign | Common Cause | Distribution Pattern |
|---|---|---|
| Redness & swelling | Bacterial or fungal infections | Ventral scales, pressure points |
| Fluid-filled blisters | Pseudomonas, wet substrates | Generalized or focal regions |
| Edematous scales | Ophidiomyces ophiodiicola | Localized thickening, raised lesions |
Diagnosing snake skin infections starts here: recognizing that these visible changes aren’t cosmetic issues but urgent skin conditions demanding your attention and veterinary evaluation for proper edema treatment.
Ulcers, Crusting, and Scale Damage
When you spot circular, oozing sores along your snake’s belly, you’re looking at ulcer treatment territory—a stage where bacterial or fungal infections have breached the scales. Snake skin infections advance from superficial crust formation to full-thickness scale erosion, exposing raw tissue beneath.
Ophidiomycosis produces those signature crusty dermatitis patches, while bacterial dermatitis management demands swift action before skin lesions deepen into life-threatening skin conditions requiring specialized reptile dermatology intervention.
Foul Odor and Discharge
When a sickly sweet or rotting stench rises from your snake’s skin lesions, you’re witnessing bacterial overgrowth that demands immediate attention. Purulent discharge—thick, cloudy exudate oozing from infected scales—signals a severe snake skin infection with a genuine risk of septicemia.
A sickly sweet or rotting odor from your snake’s skin signals severe bacterial infection demanding immediate veterinary attention
Watch for these malodorous lesions indicating infectious diseases:
- Caseous oral pus with a distinctly sour, foul smell
- Blood-tinged mucus from progressing fungal infections
- Necrotic scale exudate marking tissue breakdown
- Fibrinous drainage correlating with systemic spread
Correct husbandry stops most infection signs before odor develops.
Distinct Margins Between Healthy and Diseased Skin
One hallmark of fungal infections and bacterial dermatitis is the sharp demarcation where diseased tissue meets healthy scales. You’ll observe clear lesion border dynamics: dull, thickened crusts contrasting with glossy, intact skin.
Scale erosion patterns often create stepped edges—73% of affected grass snakes showed margin erosion—making skin lesion mapping straightforward during your examination and enabling precise tracking of dermatitis progression.
Differentiating Infection From Other Skin Issues
Not every skin issue your snake develops stems from infection. Traumatic injuries, shedding complications, genetic conditions, and husbandry problems can all mimic infectious disease, making accurate differentiation essential for appropriate treatment.
Understanding these distinctions helps you avoid misdiagnosis and ensures your snake receives the care it actually needs.
Normal Shedding Versus Infection
When evaluating skin lesions on your snake, distinguish normal shedding patterns from infection signs by examining the timing, appearance, and progression of changes. Healthy ecdysis produces uniform dullness and complete skin removal within seven to fourteen days.
Fungal infections and bacterial dermatitis create persistent focal ulcers, malodorous discharge, and erythema that worsen despite proper snake hygiene.
Dysecdysis causes often predispose snakes to secondary skin conditions requiring reptile dermatology assessment.
Traumatic Injuries and Genetic Disorders
Traumatic lesions from abrasive substrates or enclosure furnishings display sharply demarcated edges along single scale rows, contrasting with the irregular expansion typical of snake skin infection. Trauma prevention through smooth substrates supports proper healing, whereas secondary infection transforms simple skin lesions into progressive dermatitis within seven to fourteen days.
You’ll recognize genetic predisposition in certain morphs showing chronic skin conditions despite ideal snake husbandry—inherited disorders affecting scale regeneration and barrier integrity require reptile dermatology evaluation.
Environmental and Husbandry Factors
Your snake’s enclosure itself can be the silent culprit behind recurring skin infections. Humidity control between 50–75%, stable temperature gradients of 20–35°C, clean substrate quality, and thoughtful enclosure design form the backbone of reptile care and management.
Poor hygiene practices—wet bedding, infrequent cleaning—create ideal conditions for bacterial and fungal snake health issues, transforming minor irritation into progressive dermatitis requiring veterinary intervention.
Recognizing Parasitic Versus Infectious Signs
Beyond the substrate and temperature you’ve perfected lies another diagnostic challenge: distinguishing live ectoparasites from deeper infectious disease.
Skin lesion analysis reveals that mite infestations produce clusters of pinpoint hemorrhages around the eyes and vent with visible moving specks, whereas fungal or bacterial skin infections generate more diffuse plaques and tissue invasion without motile organisms—parasite identification demands close inspection for successful infectious disease management.
Diagnostic Techniques for Snake Skin Infections
When you suspect your snake has a skin infection, getting an accurate diagnosis isn’t something you can do with a quick glance. Your veterinarian will use a combination of hands-on examination and laboratory techniques to pinpoint exactly what’s causing the problem.
Let’s walk through the diagnostic methods that help distinguish one type of infection from another.
Physical Examination and Visual Assessment
Your first line of defense in identifying snake skin infection starts with a thorough integument exam from head to tail. Visual inspection reveals telltale skin lesions—erythema, ulcers, blistering, or crusting—that signal dermatologic evaluation is needed.
Ultraviolet screening can improve detection, with 86% sensitivity for ophidiomycosis. Systematic dermatology and skin conditions assessment, including checking ventral scales and facial regions, ensures you won’t miss early snake skin problems.
Skin Scraping and Microscopy
Once you’ve spotted suspicious skin lesions, diagnostic techniques shift to hands-on microbiology. Skin scraping with a scalpel blade captures epidermal debris, parasites, and fungal elements for microscopic analysis.
You’ll transfer material to a slide with mineral oil to detect mites, bacterial rods, or hyphal structures—simple first-line tests that guide deeper workups.
Multiple scrapings from active lesion edges improve parasite identification and fungal detection sensitivity when diagnosing snake skin infection.
Fungal Cultures and Identification
When microscopy raises suspicion for fungal disease, you’ll want to pursue fungal isolation using standard diagnostic protocols. Swab or biopsy the lesion, then inoculate Sabouraud-based culture media at 30 °C.
Identification methods—colony morphology and molecular typing—pinpoint Ophidiomyces ophiodiicola, the agent behind snake skin infection. These microbiology techniques clarify which fungal infection you’re truly facing.
Advanced Imaging for Complicated Cases
When physical examination and fungal culture can’t determine full lesion extent, radiography offers an initial view, though CT scanning and MRI techniques provide enhanced soft tissue detail. Ultrasonography detects subcutaneous edema and abscesses beneath diseased scales.
In refractory skin infections, nuclear imaging reveals metabolically active foci before structural changes appear, guiding treatment options for snake infections you might otherwise miss.
Management and Treatment of Skin Infections
Once you’ve diagnosed a skin infection in your snake, the next step is implementing a treatment plan that tackles both the immediate infection and the underlying factors that allowed it to develop. Successful management requires a combination of appropriate medications, environmental corrections, and ongoing veterinary oversight.
Let’s look at the essential components of treating and preventing snake skin infections.
Topical and Systemic Medications
When treating fungal infection, you’ll often encounter medication resistance in bacterial isolates—two-thirds showed resistance to amoxicillin–clavulanate in one study, making third-generation cephalosporins your best systemic option.
Topical antifungals like miconazole work well for localized lesions when paired with wound management, while itraconazole or voriconazole address deeper dermatomycoses. Treatment outcomes improve dramatically when you combine targeted antifungal therapy with proper veterinary diagnostic techniques and environmental correction.
Supportive Care and Husbandry Improvements
Beyond medications, you must address the environmental deficiencies that allowed infection to take hold. Correcting husbandry forms the cornerstone of recovery—over 80% of dermatologic cases required temperature adjustments, and proper thermal gradients shortened healing by 25–30%.
Focus on these evidence-based interventions for superior snake care and veterinary care for snakes:
- Thermal Support: Maintain species-specific preferred temperatures within 2–3°C to boost immune function by up to 40%
- Humidity Management: Keep relative humidity at 50–60%, avoiding persistently saturated conditions that fuel ventral scale dermatitis
- Enclosure Hygiene: Disinfect weekly and spot-clean within 24 hours to limit bacterial proliferation
- Nutritional Therapy: Secure adequate vitamin A and balanced calcium levels to support epithelial integrity
- Environmental Monitoring: Use digital thermometers and hygrometers at multiple points to verify consistent conditions
Replace damp substrates with easily disinfected materials like paper during treatment, and provide lukewarm soaks for 20–30 minutes daily when dysecdysis complicates skin lesions. Isolation of affected individuals prevents transmission of contagious pathogens like Ophidiomyces, while daily visual inspections let you track lesion progress and adjust reptile care and management protocols accordingly—proper animal husbandry isn’t optional when treating snake skin conditions.
Preventive Measures for Skin Health
Prevention surpasses even the most aggressive treatment regarding skin infections. Rigorous biosecurity measures are essential to safeguarding reptile skin health.
You’ll achieve this through quarantine protocols, isolating new arrivals for 60–90 days, maintaining humidity at 50–60%, and weekly enclosure disinfection with 10% bleach solutions held for 60-second contact times.
Environmental control and hygiene practices directly reduce fungal disease management challenges and dermatology and skin conditions, protecting snake skin before intervention becomes necessary.
Veterinary Monitoring and Follow-Up
Structured veterinary care demands recheck intervals every 7–14 days initially, then biweekly until lesions resolve. You’ll monitor treatment outcomes through repeat skin scrapings and clinical monitoring of lesion depth, crusting, and secondary infection.
Drug safety assessments—watching for anorexia or weight loss—protect snake health during systemic therapy.
Long-term surveillance extends months beyond apparent cure, because ophidiomycosis can resurface when you stop too soon.
Frequently Asked Questions (FAQs)
Can snake skin infections spread to other pets?
Sure, your snake’s bacterial skin infection isn’t exactly hosting an interspecies disease party—but reptile-associated zoonotic disease transmission through Salmonella contamination and shared environments demands strict pet hygiene, reptile handling protocols, and infection control measures protecting all household animals.
How long does recovery typically take?
Recovery timeframes for snake skin infections depend on infection severity and treatment compliance. Mild bacterial dermatitis may resolve within three to six weeks, while moderate cases require several months of systemic therapy.
Fungal disease treatment often demands prolonged convalescence periods exceeding ten weeks before healing processes conclude.
Are certain snake species more susceptible?
Yes—taxonomic patterns reveal striking differences. Water-associated genera like Nerodia and Natrix face elevated fungal disease prevalence, while crotalids show severe host–pathogen interactions.
Environmental risks and genetic factors shape species susceptibility more than you’d expect.
What humidity levels help prevent skin infections?
You’ll want to maintain 55–75% relative humidity for most boas and pythons, allowing enclosures to dry between misting.
Prolonged dampness encourages bacterial and fungal growth, while inadequate moisture causes incomplete sheds and secondary skin infections.
Can humans contract infections from infected snakes?
While snake fungal disease itself isn’t zoonotic, snakes carry Salmonella—affecting over 60% in captivity.
Direct handling and environmental contact create transmission pathways, requiring rigorous handwashing and habitat hygiene to prevent human infections.
Conclusion
An ounce of prevention beats a pound of cure regarding your snake’s integumentary health. Recognizing snake skin infections before they spiral into systemic crises hinges on your vigilance—catching that first erythematous margin, that subtle textural shift, that unexplained moisture retention.
You’ve now got the diagnostic framework to distinguish pathology from physiology, to act decisively, and to preserve your animal’s dermal integrity before complications demand aggressive intervention.
- https://www.nature.com/articles/s41598-024-55354-5
- https://www.in.gov/dnr/fish-and-wildlife/wildlife-resources/animals/snakes/snake-fungal-disease/
- https://en.wikipedia.org/wiki/Ophidiomyces
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7544097/
- https://www.vetlexicon.com/exotis/reptiles/parasitology/articles/necrotizing-dermatitis/